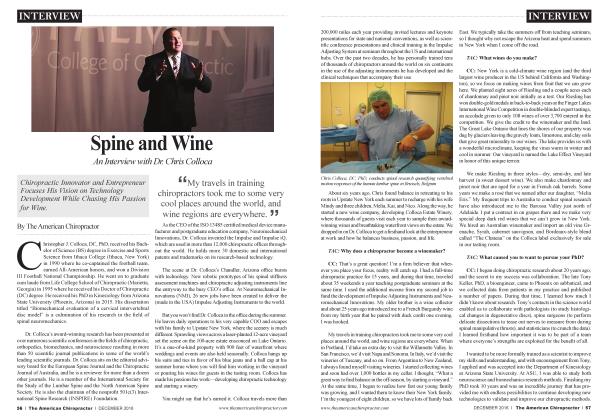
Requirements for Chronic Pain Therapy
REHAB
Bill Landtbom
After a successful treatment, do any of your patients walk toward the door and spin around to thank you? You know right then the patient would regress to his or her old postural habits, returning in a lesser condition than you expected. Every mother told her kids to “sit up straight,” again and again. She was right, but did her kids listen? Instead, they’ve gone through life with poor spinal mechanics compromising the health of their lumbar spines to where those habits become innate.
We know correct spinal mechanics—we’re in the business—but we typically use our lumbar spine as the default joint enabling us to get closer to an object. When we bend, reach, or twist, we begin with spinal flexion, rather than another joint that could reach the object without compromising correct posture. Every such repetitive motion weakens the disks, leading to ultimate failure. A study by Punnett, Fine, Chaffin, et al,1 stated that “Back disorders and non-neutral trunk postures of automobile assembly workers” found a “strongly negative” effect for those continuing spinal flexion. However, spinal flexion is a behaviorally acquired habit, so, like a long-term smoker, it must be corrected in the same way.
A Harvard Medical School paper2, found that a curved, Ann surface against the spine provided behavioral impetus through proprioception, to lessen the postural regression. Instead of initiating movement consciously, the spinal tissues assume control, reorienting then positioning and staying within a safe range of motion, simply because it feels better that way! Proprioception is the behavioral solution. Finally, like many habits, a wearable unit with these benefits is imperative so that the behavior change is continuous, until anew, collect muscle memory is created. What’s tlie point of waking up after a night on a perfect ergonomic mattress and immediately revert to old spinal habits for the rest of the day?
“Have you ever been frustrated when several treatments do not attain the desired outcome? The reason is simple: postural regression between appointments. ÏÏ
Have you ever been frustrated when several treatments do not attain the desired outcome? The reason is simple: postural regression between appointments. The solution is the same. This proprioceptive environment reinforces new and collect muscle memory behaviorally and continuously. Once that kicks in, this new habit is present whether feeling the “curved, Ann surface” or not.
If the patient still stops improving, typically the pain from past damage compromises functional form in rehab exercises. Toxic pharma is one intervention for beneficial rehab, but at too high a risk. Instead, certain magnets have been proven to contain painrelieving benefits. Not just any magnet, though. Most magnets aie “spot magnets” similar to refrigerator magnets, with a magnetic field the exact size/shape of the host magnet, emanating a field 90 degrees from the host. Wherever there is no magnet, there is no magnetic benefit. “Therapeutic” magnets, covering the entire lumbar area (1) increase blood flow, (2) shrink inflammation, which reduces pressure on the nerves and tissues, and (3) in some cases, actually block pain signals to the brain. Your patient performs rehab protocols with no postural regression, leading to an earlier “prognosis” where surgery becomes a very poor option.
F or non-chronic patients, magnets may not be required, but any device that can collect spinal mechanics and create new muscle memory will get faster resolutions than any other protocol without those benefits.
To sum up, the requirements for successful spine injury rehab (i) maintain functional form during exercises, (ii) create new muscle memory to resist future postural regression, (while wearing the device or not) and minimizing pain from prior damage to accelerate tlie healing process. This will lead to more conservative treatment results, that keeps patients in your practice where they belong!
References
1. Steven J Lipson, “Orthotic Considerations in the Management of Low Back Pain”
2. Scandinavian Journal for Work and Environmental Health
Several years ago, I was rear-ended while driving, and it blew two discs. Within three days, the sciatic pain was unbearable and I could barely walk. I went to an MD, a DO, and a DC, to no avail. Knowing that pressing my curved spine against a wall (flat) helped a little, I shaved some Styrofoam to follow my spine curve, snugged up with a belt around my waist, and immediately felt better I made a prototype, wore itfor two years, and showed up at the hospital two years after the accident for surgery (auto accident—insurance company wanted the case closed). Before surgery, the surgeon ordered an MPT because I was golfing and skiing when, to him, I could barely walk. While on the operating table, the surgeon came in and said, “Eve never seen this in all my years of surgery, but you’re going home! ” The disc fragments had “resorbed”—a true ‘‘conservative ” outcome. (During the two years between the accident and the surgery date, I did see a chiropractor, so I do give her some credit, but even she acknowledged early on that surgery was the only option). You can reach Bill at 415-387-4082 or go to the website www.backaline.com
 View Full Issue
View Full Issue