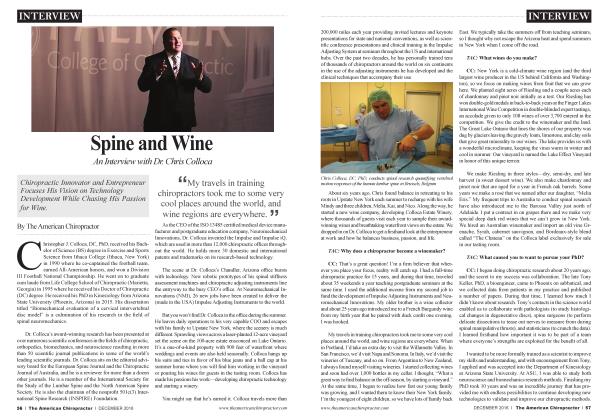
Scar Formation May Be Hindering Your Patients’ Outcomes
REHABILITATION
Ed Le Cara
Scar formation is a natural part of the woundhealing process. Scars are formed by fibrous connective tissue assisting wound repair in the skin and other body tissues. Scars are formed on the skin, underlying tissue, and internal organs where an injury occurred, an incision was made, some part of the body was cut, or a disease infected and caused damage to the tissue. The damaged tissue is replaced by scar tissue to maintain the normal body processes (Waibel & Rudnick, 2015), but scar tissue is unlike normal tissue and may cause pain and limitations in motion, thus needing medical intervention.
Effects of scars on movement and pain:
Organs and muscles work through a series of movements or swings. Scar formation on organs or muscles can alter the way the tissue moves. Movement is altered around a scar because the flexibility of the scar tissue is different from that of the normal tissue. A scar’s limited flexibility leads to a limited range of motion. Scar tissue may limit muscle layers and connective tissue, causing different degrees of discomfort and pain. The scar tissue is weak and less elastic. It is vulnerable to reinjury, compared to normal tissue, and it can easily lead to chronic pain. Treatment is advisable to allow normal tissue mechanics and to cosmetically improve the appearance of scar tissue (Rice, et ak, 2014).
A common example of scar tissue formation is the rectus abdominis muscle fibers, which are routinely cut during abdominal surgery (i.e., C-section, Figure 1; or hiatal hernia, Figure 2). Rectus abdominis needs to stretch in order to allow spine extension in the case of movements such as arching your back in a volleyball spike (Kerwin, Tal, Kader, Stiff, & Fakhouri, 2014). The limitations on movement due to the scar formation on the anterior aspect of the body can
lead to dysfunction and pain on the opposite side by limiting global range of motion.
A surgery on internal organs produces visceral adhesions and scar tissue that affects the nor-
^The longer the scar has been around, the longer the treatment will takeJ J
mal functioning of the organ. This is because organs have a connection to other organs and soft tissue. The presence of scar tissue around these organs causes pain and musculoskeletal dysfunction due to limitations in flexibility. A good example of this is the gallbladder. The gallbladder is connected to the common bile duct and pancreas. The bile duct and pancreas are facially linked with the diaphragm, which is connected to the rib cage (Kligennan, 2014). Performing a surgery involving these organs will produce scar tissue that may limit breathing (limiting rib cage expansion) and the functionality of the rib cage, causing musculoskeletal
imbalance and possibly pain.
Smaller forms of scar tissue are called adhesions. Adhesions cause an inability of tissue to glide and slide over one another, resulting in stiffness and reduction in strength and range of motion. Adhesions are thought to limit nerve gliding. The nerves become entrapped in the tissue instead of being able to slide through the muscles, which limits range of motion of the involved limb. If this occurs around the spinal column, adhered nerve roots can occur. Adhered nerve roots at the lumbar spine display symptoms similar to hamstring tightness in the back of the thigh and commonly restrict the ability to toe touch.
In general, skin scars lead to a reduction in motion and strength, pain, and discomfort. In order for a muscle to have enough power and to move appropriately, it should stretch and contract fully. The shortening and weakening effects of the skin clearly make it impossible to fully stretch and contract it to the optimum levels, and thus, motion will be limited and pain will result due to strained contraction and expansion of body tissues.
Conservative Treatment Options:
The University of Washington Orthopedic Department noted that post surgical scar tissue can reduce joint range of motion and recommends treatment to improve flexibility of
the injured tissue. Reduced range of motion can be avoided with a prescription of manual therapy and correct motion exercises to help avoid myofascial adhesions around the affected area.
Treatment of scars can be easily performed in chiropractic, massage, or physical therapy clinics. For the best outcomes to improve scar tissue flexibility, intervene as early as one can without disrupting tissue healing. Normally, two weeks post surgical is enough time. Prior to the tissue being ready to be manipulated, treatment for excessive inflammation can be helpful. Using kinesiology tape can help lift the skin to allow for fluid to move easier to the heart.
After the tissue has had enough time to mend, combine heat with lightly applied instrument-assisted soft-tissue manipulation and kinesiology taping.
Intervention Options:
Step 1. Determine which direction the tissue is not moving. Sometimes different part s of the scar aie not moving in different directions. (Figure 5)
Step 2. Use cold laser, hydrocollator pack, diathermy, or therapeutic ultrasound to wann the target tissue for 10 to 15 minutes.
Step 3. Lightly apply instrument-assisted soft-tissue manipulation for between three to five minutes depending on the size of the scar (Figure 7) into the direction of restriction.
Step 4. Cut the kinesiology tape the opposite of how one would apply for other applications—lengthwise into the tape. By cutting that way, the tape does not recoil back on itself and the tissue can be pulled into the direction of restriction. Start an inch or two on the opposite side of restriction and pull the
tissue (with the tape) into the restriction. Typically, a patient will do this at home every night before bed.
Step 5. Give patients range-of-motion exercises to do every day for the tissue to extend (i.e., stretching).
The longer the scar has been around, the longer the treat-
ment will take (up to six months). Start with two sessions per week with ample time between sessions (all discomfort gone before next session) and have the patient tape the scar at night before bed to achieve good results. Not only will the scar look like the normal skin tissue, but the patient also will experience decreased restriction in motion and a decrease in symptoms.
References
1. Rice, A. I)., Wakefield, L. B., Patterson, K., Reed, E. D. A., Wurn, B. F, King III, C. R., & Wurn, L. J. (2014). Decreasing adhesions and avoiding further surgery in a pediatric patient involved in a severe pedestrian versus motor vehicle accident. Pediatric reports, 6(1).
2. Kerwin, L. Y, Tal, E., Kader, A., Stiff, M. A., & Fakhouri, T. M. (2014). Scar prevention and remodeling: a review of the medical, surgical, topical and light treatment approaches. International journal of dermatology, 53(8), 922-936.
3. Waihel, J. S., & Rudnick, A. (2015, March). Current trends and future considerations in scar treatment. Seminars in cutaneous medicine and surgery (Vol. 34, No. 1, pp. 13-16). Frontline Medical Communications.
4. Kligerman, A. E. (2014). U.S. Patent Application No. 14/446,779.
Ed Le Cara, DC, PhD, MBA, ATC, CSCS, has worked in private practice, Veteran ’s Administration Hospital, LUlc^ corPorate America (24 Hour Fitness) helpingpeopie improve human movement for more than 16 years. He is the owner of KinetikChainDenver.com and the director of research at RockTape. You can contact Ed by e-mail (edfiKinetikChain. com) or TwitterZlnstagram: (cfdrlecara.
 View Full Issue
View Full Issue