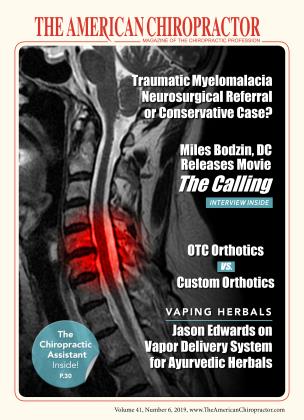
Traumatic Myelomalacia
FEATURE
Diagnosis & Collaborative Management Between the Chiropractor as the Primary Spine Care Provider and the Neurosurgeon
Matt Erickson DC
Mark Studin DC
John Edwards MD
Clay Wickiser DC
Neurosurgeon
Myelomalacia is defined as softening of the spinal cord, which can be a result of injury and represents a serious and potentially life-threatening sequella to injury if not treated. According to Zhou, Kim, Vo, and Riew (2015), “Cervical myelomalacia is a relatively uncommon finding on MRI, with an overall prevalence of 4.2% among all patients who underwent cervical MRI. Males had a higher prevalence (5.6%) than the females (3.0%).”pE250
The authors also reported, “There were considerable variations in the prevalence of myelomalacia in patients referred by different specialties/subspecialties. Specialists in spinal cord injury had the highest rate (28.7%), followed by neurological (8.4%) and orthopedic (6.4%) spine surgeons, general neurosurgeons (5.5%), and neurologists (4.2%). Specialists who generally do not treat patients with spine problems had the lowest (1.2%) followed by non-spine orthopedists (1.6%) and primary care doctors (2.1%).” pE248
Platt, McConnel, and Bestbier (2006) reported, “Myelomalacia is ischemic or hemorrhagic necrosis of the spinal cord that can occur following acute spinal cord injury, and represents extensive damage of the intramedullary spinal vasculature.” 3'p 78 According to Lu, Lamb, and Targett (2002), “In small animal neurology, the term myelomalacia ... is normally used to refer to hemorrhagic infarction of the spinal cord that can occur as a sequel to acute injuries, such as that caused by intervertebral disc extrusion. Myelomalacia may occur as a focal lesion or may spread cranially and caudally along the spinal cord, resulting in a diffuse, severe lesion. Histologic lesions of myelomalacia are compatible with ischemic necrosis.”2"p 326
According to a website article titled, “Myelomalacia” by Foster and Wilborn (2019), “Myelomalacia is a medical condition in which the spinal cord becomes soft. It is caused by the insufficient blood supply to the spinal cord, either as a result of bleeding or because of poor circulation. Myelomalacia most often occurs as a result of the injury.” (www.wisegeek.com/what-is-myelomalacia.htm) Foster and Wilborn (2019) added, “Caused by mild to severe spinal cord injury, myelomalacia leads to neurological problems, often related to muscle movement. Often, the onset of the condition is slow and subtle, making it difficult for doctors to catch at an early stage. While symptoms vary, they may include loss of motor function in the lower extremities, sudden jerking of the limbs, an inability to sense pain, depression, difficulty breathing, and paralysis. The damage can migrate towards the brain in a condition known as ascending syndrome. Myelomalacia can be fatal if it causes paralysis of the respiratory system.” 4
Platt, McConnel, and Bestbier (2006) also reported, “The exact pathophysiology is poorly understood but it seems to be the result of the concussive effects of trauma, ischemia, and the release of vasoactive substances, oxygen-free radicals and cellular enzymes. When the spinal cord is acutely damaged, cell death in the gray matter may occur within 4 hours, with this area of necrosis expanding for a few days.”3'ps 78 This means that many patients can have significant underlying progressive pathology with symptoms that have not yet fully expressed themselves, but the evidence is demonstrative to the trained expert. This evidence further supports the necessity and importance of having a primary spine care provider with trauma qualifications to diagnose the issue early on and coordinate care with the neurosurgeon.
Operative Neurosurgery, “Myelomalacia” (administrator updated) (2018), explains that, “Gradual cranial migration of the neurological deficits (problems relating to the nervous system), is known as ascending syndrome and is said to be a typical feature of diffuse myelomalacia. Although clinical signs of myelomalacia are observed within the onset (start) of paraplegia, sometimes they may become evident only in the post-operative period, or even days after the onset of paraplegia. Death from myelomalacia may occur as a result of respiratory paralysis when the ascending lesion (abnormal damaged tissue) reaches the motor nuclei of the phrenic nerves (nerves between the C3-C5 region of the spine) in the cervical (neck) region.” (https: / / operati veneuro surgery, com/ doku.php?id=myelomalacia)
As such, it is imperative for there to be collaborative case management between the primary spine care expert and the neurosurgeon. An early diagnosis by the primary spine care provider is valuable because it identifies, treats, and involves the neurosurgeon when clinically indicated because, if left undiagnosed and untreated, myelomalacia can become a seriously debilitating and/ or life-threatening injury. Those injuries result from the trauma that the spinal cord is exposed to (auto accidents, sports injuries, falls, etc.). Currently, there is a growing body of chiropractors nationally that are primary spine care and trauma qualified and trained in the early detection (diagnosis) and management of this population of patients.
Diagnosis
According to Zohrabian and Flanders, Chapter 37: Imaging of trauma of the spine from the Handbook of Clinical Neurology Part II, “MRI is the only available imaging modality that is able to clearly depict the internal architecture of the spine cord, and, as such, has a central role in depicting parenchymal changes resulting from injury.” p 760 Further, “It may be difficult to distinguish spinal cord white matter from gray matter, especially in the sagittal plane, due to the similar T1 and T2 relaxation characteristics. Many prior investigations have shown that MRI characteristics of (SCI) Spinal Cord Injury, including presence and extent of cord edema and hemorrhage, are concordant with neurologic impairment at the time of injury and predict recovery.” p760
Zohrabian and Flanders also wrote, “The most common location of posttraumatic spinal cord hemorrhage is the central gray matter of the spinal cord at the point of mechanical impact. The lesion most often represents hemorrhagic necrosis; true hematomyelia is rarely encountered. The lesion appears as a discrete focus of hypointensity on T2-weighted and gradient echo images, developing rapidly after SCI.” 6'p-760
Zohrabian and Flanders added, “Moreover, the location of cord hemorrhage has been shown to closely correspond to the neurologic level of injury, with frank hemorrhage correlation with poor neurologic recovery.” p760
Further, “Although several MRI classification schemes have been proposed, there are three common imaging observations: spinal cord hemorrhage, spinal cord edema, and spinal cord swelling. Each of these characteristics can be farther described by their rostral-caudal (top to bottom) location in the cord and the amount of cord parenchyma they involve. ”p 760
“Spinal cord edema, colloquially referred to as a cord contusion, can occur with or without hemorrhage. Edema involves a length of the spinal cord above and below the level of injury, with the length of the spinal cord show to be proportional to the degree of initial neurologic deficit. Spinal cord hemorrhage always coexists with spinal cord edema. Cord edema alone usually confers a more favorable prognosis that cord hemorrhage. ”p-761
According to D.J. Seidenwurm MD (for the Expert Panel on Neurologic Imaging), “/n traumatic myelopathy, the first priority is mechanical stability. Plain radiographs are sometimes useful for this purpose, but CT is more useful when a high probability of bony injury or ligamentous injury is present. In many centers, routine multidetector CT with sagittal and coronal reconstructions has replaced plain radiographs, especially in the setting of multiple trauma.” p 1032
Concerning CT, Foster and Wilborn (2019) reported, “Myelography uses a contrast medium injected into the spine to reveal injuries in x-rays. It is more invasive than an MRI but can also detect injury in some cases in which MRI cannot. Therefore, myelography is typically used as a follow up to MRI when the latter fails to identify the source of pain or injury. ” 4
Finally, Zohrabian and Flanders reported, “Unlike in spinal cord cysts, myelomalacia will not parallel CSF (cerebral spinal fluid) signal intensity and its margins will usually be irregular and ill-defined (Falcone et al., 1994). The cord may be normal in size, although it is frequently atrophic at the site of myelomalacia (Fig. 37.24)” P763
Zhou, Kim, and Vo (2015) further explain, ‘Myelomalacia is a radiographical finding on magnetic resonance imaging (MRI) manifested by an ill-defined area of cord signal change, visible on Tland T2-weighted sequences as hypoand hyperintense areas, respectively. It is commonly associated with focal cord atrophy. It occurs as a sequel to spinal cord injury (SCI) due to different causes such as cord compression, ischemia, and hemorrhage. It is the most common finding in patients with previous spinal cord injury with a prevalence of 55% among patients with SCI.” E248
Management
Due to the seriousness and progressive nature of myelomalacia, it is important for the chiropractor, as the Primary Spine Care Provider to recognize the signs and symptoms associated with myelomalacia and to identify the lesion on MRI and, if identified, to immediately refer the patient for a neurosurgical consultation. This also underscores why physical therapists, although licensed to treat the spine, should never be the first provider to manage a spinal case, as diagnosing such cases and other conditions are not within their scope.
Foster and Wilborn (2019) reported, “Unfortunately; neurological damage due to myelomalacia is permanent. It can also worsen, as the nerve damage can cause affected muscles to whither. Treatment is focused on preventing further damage. Possible treatments include spinal cord surgery and medication with steroids, which serves to relax spastic muscles, reduce pain, and reduce swelling of the spinal cord” They also suggested that, “Stem cell therapy may be used to repair neurological damage caused by myelomalacia in the future, but the therapy is currently experimental and controversial. Recent technology suggests that adult stem cells, which can be harvested from the patient’s own body, show promise in treating neurological damage by allowing new, healthy tissue to grow. ” (www.wisegeek.com/what-is-myelomalacia.htm)
Zhou, Kim, Vo, and Riew (2015) reported that, “The presence of myelomalacia in the cervical spinal cord has prognostic value after decompression surgery. Some surgeons consider operative treatment of all patients with myelomalacia based on the assumption that myelomalacia is a relatively uncommon finding. ”(ps E248) The authors also observed that, “Many patients with myelomalacia are clinically asymptomatic or have only mild myelopathic symptoms and signs. The extent of intramedullary changes on MRI does not always correlate with clinical symptoms. Hence, for patients with asymptomatic or mild myelopathy with myelomalacia on MRI, the appropriate management remains controversialp E249
Zhou et al. (2015) added, “Several articles have suggested that conservative management is not an unreasonable option for patients with myelomalacia and mild myelopathy. It has been reported that the condition of 56% of patients with mild CSM (cervical spine myelomalacia) had not deteriorated or required surgery after 10 years. However, 2 of 45 (4.4%) patients who were treated nonoperatively with T2 hyperintensities experienced catastrophic neurological deficits with trivial trauma. Early-stage myelomalacia may be reversible, depending on the severity of the initial SCI (spinal cord injury), and may be reversed after decompression surgery. ” p E249
This is not to suggest that surgery for myelomalacia is always required. According to Dr. Mark Kotter in a website article titled “Myelomalacia” from myelopathy.org, “The presence or absence of myelomalacia should not be used to define when surgery should occur. ” Although he stated, “Its presence and extent may be related to prognosis(http://www.myelopathy.org/myelomalacia.html) Myelomalacia, like any spinal-related injury never uses imaging findings exclusively as an arbiter for surgery. That decision is reserved for combining a clinical examination with imaging findings and the surgeon decides if surgery will benefit the patient. It is the role of the primary spine care provider to ensure and early diagnosis and referral to try to develop treatment protocols to surgically decompress the spinal cord to help reverse this pathology and often can be done if damage has been minimized.
Surgery for Myelomalacia
Patients with myelomalacia may require surgery to decompress the spinal cord. Different techniques are used depending on the pathology that may or may not include spinal fusion. Many patients are treated with an anterior approach. The offending material is removed, and the spine is reconstructed either with a fusion or an artificial disc replacement. Some patients, especially with multilevel pathology, require posterior decompression with or without fusion.
The primary goal of surgery for myelomalacia is to decompress the spinal cord. Secondary goals include maintaining spinal structural integrity, alignment, and biomechanical function.
Biomechanical Management
Concerning surgically balancing the spine, sagittal (front to back) balance is associated with better post-surgical outcomes. Healia. com reported on lectures by Serena Hu, MD; Jean Charles LeHuec, MD, PhD; and J.N. Alastair Gibson, MD, FRCS(Ed), FRCS (Tr &Orth), MFSTEd related to outcomes of lumbar spine surgery and sagittal balance. According to Dr. Hu, “Surgical outcomes for spine surgery are improved when spinal, pelvic and hip alignment is considered in both degenerate and deformity cases, and how we better understand these will help us better improve outcomes for our patients
Dr. Hu further commented, “Sagittal imbalance in a patient can negatively affect the outcomes of a surgical procedure. But, how extensive the surgery required is to correct the imbalance must be carefully considered for the individual patient, according to Hu.” Dr. LeHuec added, “Sagittal balance is an active phenomenon for patients. The best course of action is to strive to achieve sagittal balance in patients. ” (https://www.healio.com/ spine-surgery/lumbar/news/print/ spine-surgery-today/%7B54ac5ca27939-407d-96a5-31 fa9c0fc904%7D/ proper-sagittal-balance-may-correlate-with-better-surgical-outcomes)
In a study by Tang, Scheer, Smith, Deviren, Bess, Hart, Lafage, Shaffrey, Schwab, and Ames (2015), they concluded, “Our findings demonstrate that, similar to the thoracolumbar spine, the severity of disability increase with positive sagittal malalignment following surgical reconstructionS21
In an article by Yeh, Lee, Chen, Yu, Liu, Peng, Wang, and Wu (2018), they concluded, “The results of this study support previous findings that functional outcomes are closely associated with sagittal radiographic parameters in the patients with the degenerative thoracolumbar spinal disease who received long-segment fusion. The achievement of global and regional sagittal balance is a crucial factor for improved postoperative functional outcomes.”p 1361
The chiropractor, as the primary care spine provider and the neurosurgeon can work together to best achieve spinal alignment and balance. If the patient has been cleared for mechanical treatment, the primary care spine provider can work to balance the spine (front to back and side to side) before any necessary surgical intervention. The neurosurgeon can work to maintain and improve spinal alignment with surgery. Post-operatively, ongoing chiropractic spinal adjustments can help maintain and continue to improve spinal alignment, which can lead to the best possible surgical outcomes.
Patients with myelomalacia present an ideal opportunity to further the relationship between the chiropractor as the primary care spine provider and the neurosurgeon. The finding of myelomalacia requires surgical consultation. If the chiropractor identifies myelomalacia, he or she can then refer to the neurosurgeon and begin the discussion necessary for further co-management. The chiropractor can ask if surgery is necessary. If so, the chiropractor can ask if mechanical treatment can be done pre-operatively or ask if it should wait until after surgery. If the patient needs close monitoring over time, the astute chiropractor can regularly check on and provide education to the patient under the direction of the neurosurgeon.
In patients with myelomalacia, the ability of the chiropractor to monitor symptoms, prepare a patient for surgery, and manage the spine mechanically after surgery are advantageous to the surgeon, who can spend more of their time performing surgery and also enjoy greater patient satisfaction and outcomes.
Conclusion
Myelomalacia represents a softening of the spinal cord that commonly results from trauma. If myelomalacia is observed on imaging, the advanced trained Doctor of Chiropractic in the capacity of a primary spine care provider should refer the patient for a neurosurgical consultation. In the event surgery is not indicated, the chiropractor can create a treatment plan with the surgeon to help axially balance and stabilize the spine, thereby reducing the compressive forces on the spinal cord and maintaining spinal mechanics. If surgery is required, the chiropractor can coordinate conservative care with the surgeon to help biomechanically balance and then manage the patient’s spine to promote a better long-term post-surgical outcome. Whether surgical or not, the chiropractor can play an integral role in the patient’s care. If the chiropractor has additional training in MRI Spine Interpretation, Spinal Biomechanical Engineering, and/or other advanced spinal knowledge, it provides the basis for better collaboration.
Mark Studin, DC, FASBE(C), DAAPM, DAAMLP, teaches MRI spine interpretation, spinal biomechanical engineering, and triaging trauma cases. He is the president of the Academy of Chiropractic teaching doctors of chiropractic how to interface with the medical and legal communities (www. DoctorsPIProgram.com) and teaches MRI interpretation and triaging trauma cases to doctors of all disciplines nationally (www.TeachDoctors.com). [email protected] or at 631-786-4253.
Dr. Erickson is the President of Body Right Chiropractic in Clearwater, Florida. He is a Palmer graduate and earned the President's List Award for clinical excellence. Through the Academy of Chiropractic, he has become Trauma Qualified, Primary Spine Care Qualified and Interprofessional Hospital Qualified. In 2018, Dr. Erickson completed a 2-year Fellowship in Spinal Biomechanics and Trauma.
John Edwards is a neurosurgeon practicing in Provo, Utah. He completely medical school at the University of Iowa and neurosurgery residency at Indiana University. He specializes in minimally invasive and complex spine surgery.
Clay Wickiser, D.C. is a 1996 graduate of Life University. He currently is in private practice in Anderson, S.C.
References
1. Zhou Yihua, MD, PhD, Kim D. Sang, MD, Vo Katie, MD, and Riew K Daniel, MD. (2015). Prevalence of Cervical Myelomalacia in Adult Patients Requiring a Cervical Magnetic Resonance Imaging. Spine, 40(4), E248-E252.
2. Lu D, Lamb CR, Targett MP. Results of Myelography in Seven Dogs with Myelomalacia. (2002). Veterinary Radiology and Ultrasound, 43(4), 326-330.
3. Platt R. Simon, McConnel J. Fraser, Bestbier Mark. (2006). Magnetic Resonance Imaging Characteristics of Ascending Hemorrhagic Myelomalacia in a Dog. Veterinary Radiology and Ultrasound. 47(1), 78-82.
4. Foster Niki and Wilbom C. (Ed). (2019, March 12). What is Myelomalacia? Retrieved from www.wisegeek. com what-is-myelomalacia. htm
5. “Myelomalacia ” (2018, June 6). Operative Neurosurgery. Retrieved from operativeneurosurgery, com/doku. php? id=myelomalacia.
6. Zohrabian, Vahe M., and Flanders, Adam E. (2016). Chapter 37: Imaging of trauma of the spine. Handbook of Clinical Neurology Part II, 136, 747-767.
7. Seidenwurm D.J., MD (for the Expert Panel on Neurologic Imaging). (2008). Myelopathy—A CR Appropriateness Criteria. American Journal of Neuroradiology, 29 (5) 1032-1034.
8. Shields Christopher B., Shand Ping Yi, and Shields Lisa B.E. (2012). Chapter 22: Post-traumatic syringomyelia: CSF hydrodynamic changes following spinal cord injury are the driving force in the development of PTSM. Handbook of Clinical Neurology, 109, 355-367.
9. Al-Shatoury Hassan Ahmad Hassan, MD, PhD, MHPE, Galhom Ali Ayrnan, MD, PhD, Benbadis, R. Selim (Ed). (2017, Nov 10). Syringomyelia. Retrieved from emedicine.medscape. com article 1151685-overview.
10. Roser Florian, Ebner Florian H, Sixt Carolin, Muller Jennifer v. Hagen and Tatagiba Marcos S. (2010). Defining the line between hydromyelia and syringomyelia. A differentiation is possible based upon electrophysiological and magnetic resonance imaging studies. Acta Neurochirugica, 152, 213-219.
11. Marla Jose Garda Antelo, Teresa Lema Facal, Tamara Pablos Sanchez, Marla Soledad Lopez, Facal and Eduardo, Rubio Nazabal Man-In-The-Barrel. (2013). A Case of Cervical Spinal Cord Infarction and Review of the Literature. The Open Neurology Journal, 7, 7-10.
12. “Myelomalacia” (n.d.). Myelopathy.org Retrieved from http://www. myelopathy, org/myelomalacia.html.
13. Kenzo Uchida MD, PhD Hideaki Nakajima MD, PhD Naoto Takeura MD, Takafumi Yayarna MD, PhD Alexander, Rodriguez Guerrero MD, Ai Yoshida MD, Takumi Sakamoto MD, Kazuya Honjoh MD, Hisatoshi Bctba MD, PhD. (2014). Prognostic value of changes in spinal cord signal intensity on magnetic resonance imaging in patients with cervical compressive myelopathy. The Spine Journal, 14(8), 1601-1610.
14. Chang David, MD (2017, Dec 7). Understanding and Treating Myelomalacia of the Spine. Retrieved fromdrdavidchangmd.com/understanding-and-treating-myelomalacia-of-the-spine
15. “Spinal Decompression Surgery” (2013 May 13). Cleveland Clinic. Retrieved from my.clevelandclinic. org/health/articles/10874-spinal-decompression-surgery
16. Serena S. Hu, MD, Jean Charles LeHuec, MD, PhD and J.N. Alastair Gibson, MD, FRCS(Ed), FRCS(Tr & Orth), MFSTEd. (2016 Jan Feb). “Proper sagittal balance may correlate with better surgical outcomes. ” Retrieved from www.healio.com/spine-surgery hmibaU news/print/spine-surgery-today/%7B54ac5ca2-7939407d-96a5-31fa9cOfc904%o7D/proper-sagittal-balance-may-correlate-with-better-surgical-outcomes.
17. Jessica A. Tang, BS Justin K. Scheer, BS, Justin S. Smith, MD, PhD, Vedat Deviren, MD, Shay Bess, MD, Robert A. Hart, MD, Virginie Lafage, PhD Christopher I. Shaffrey, MD, Frank Schwab, MD and Christopher P. Ames, MD. (2015). The Impact of Standing Regional Cervical Sagittal Alignment on Outcomes in Posterior Cervical Fusion Surgery. Neurosurgery 76, S14-S21.
18. Kuang-Ting Yeh, MD, PhD, Ru-Ping Lee, RN, PhD, Ing-Ho Chen, MD, Tzai-Chiu Yu, MD, Kuan-Lin Liu, MD, PhD, Cheng-Huan Peng, MD, Jen-Hung Wang, MD, and Wen-Tien Wu, MD, PhD. (2018). Correlation of Functional Outcomes and Sagittal Alignment After Long Instrumented Fusion for Degenerative Thoracolumbar Spinal Disease. Spine, 43(19), 1355-1362.
19. Am merman Joshua M. MD, (2019 February 6). “Adjacent Segmental Disease and Back Pain. ” Retrieved from https://www. spineuniverse. comconditions/spinal-disordersadjacent-segm en t-disease-back-pain.
 View Full Issue
View Full Issue