The term “cytokine storm” emerged in news in the context of those people who developed a severe case of COVID-19 and required hospitalization. I have been studying cytokines for many years, but I had not read about the cytokine storm until COVID-19 emerged. In fact, the term cytokine storm has been used previously in the context of the seasonal flu as made evident in the title of this 2016 article:
Lieu Q, Zhou Y, Yan Z. The cytokine storm of severe influenza and development of immunomodulatory therapy. Cell Mol Immunol. 2016; 13(1):3-10.
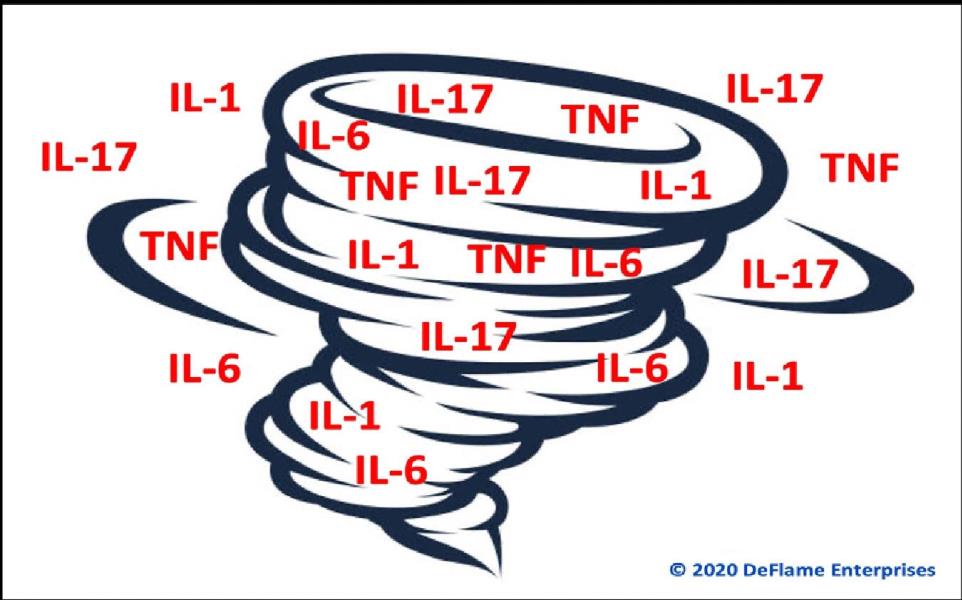
Cytokine is the name given to a family of several dozen proteins, the most notable group are called interleukins, of which there are over 30. Most cytokines are pro-inflammatory, such as interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-17 (IL-17), and tumor necrosis factor (TNF).
Cytokines are released by cells when they are stressed. After the stressor resolves, cytokine levels are supposed to go back to normal. A cytokine storm refers to an excessive release of cytokines that subsequently damages the body or leads to death. In “storm language,” a cloudy drizzly day can be likened to “catching a cold” and feeling under the weather for a few days. The cold symptoms were created by a mild elevation in the production of cytokines and other inflammatory chemicals. In contrast, a cytokine storm is like a tornado or hurricane that rips a town apart, causing death and destruction.
Cytokines are released by multiple cell types but were first identified to be released by immune cells called leukocytes, which is how the word interleukin came to be. Cytokines are released in excess in response to stressful events that are overtly traumatic such as a bee sting, spraining a joint, or an infection. The redness, heat, swelling, fever, and pain that result from these traumatic events are caused by cytokines and other pro-inflammatory chemicals.
Over the last 20 years, scientists discovered that overt trauma is not necessary to cause cells to increase their release of cytokines at a sustained chronic low level. Chronic mental/emotional stressors events, sedentary living, chronic sleep loss, and a pro-inflammatory diet can cause cells to release an excess of cytokines. Even minor acute stressful events can cause cytokine release, such as eating several donuts in one sitting or missing a night’s sleep. We should view these as lowgrade cumulative stressors, as indicated in the following image.
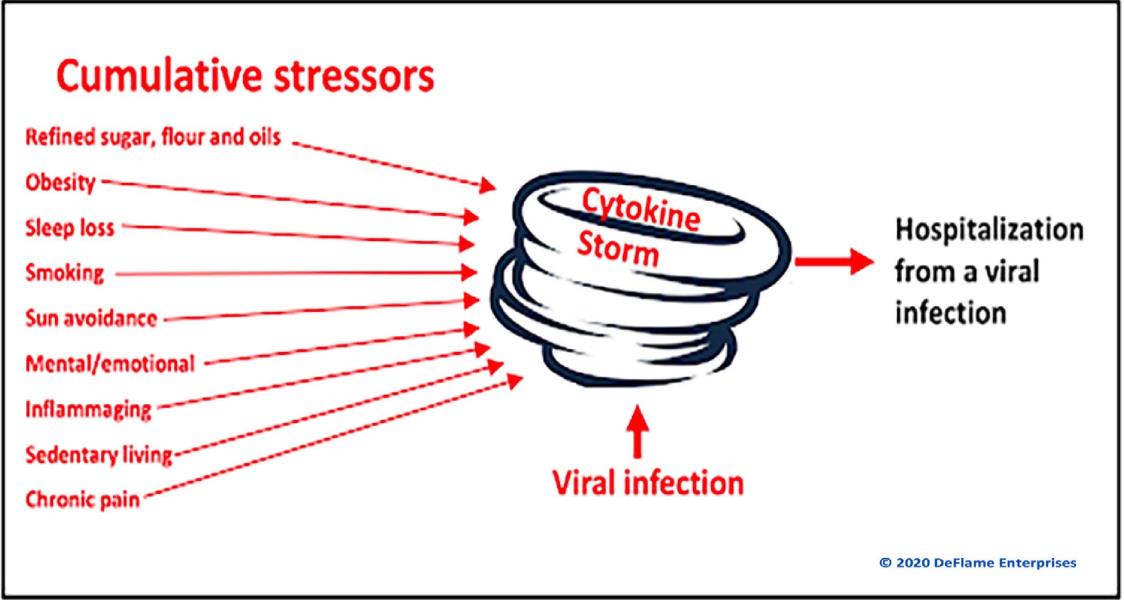
Most people who suffer from too many years of exposure to chronic stressors and the subsequent chronic inflammation will likely develop a chronic inflammatory disease, such as chronic pain, depression, diabetes, hypertension, heart disease, cancer, Alzheimer’s disease, and/or other chronic diseases. It is important to understand that these various diseases manifest because people are chronically living in an elevated cytokine state. So, it should not be surprising that when some of these people are infected by a virus, they will suffer a lethal cytokine storm. While it is possible to measure blood levels of cytokines, it is not a common practice in the clinical setting and they are expensive to measure. A pro-inflammatory protein called high sensitivity C-reactive protein (CRP) is the best option as it is inexpensive and its levels rise along with cytokines, so it mirrors cytokine production. A normal level of CRP is less than 1 mg/L. Between 1 and 3 mg/L is considered to reflect mild inflammation. The average middle-aged American has a CRP of 1.5 mg/L. It is estimated that 25% of the US population has CRP levels over 3 mg/L, which reflects a state of moderate to high inflammation. The higher the CRP level, the worse the outcome will typically be if some are injured or infected.
The practical clinical message you can deliver to your patients is this... a normal CRP level below 1 mg/L suggests that cytokine levels are also normal. The goal should be to DeFlame the diet and lifestyle to the degree that CRP levels drop below 1 mg/L. Some additional anti-inflammatory goals include getting fasting glucose well below 100 mg/dL, fasting triglycerides below 90 mg/dL, and HDL cholesterol above well 50 mg/dL for women and well above 40 mg/dL (1-3). These are very reasonable goals that almost anyone can achieve and will essentially guarantee that a cold, flu, or coronavirus infection will be a mild or a somewhat annoying experience, rather than a life-threatening event.
The primary dietary modification that most people need is to drastically reduce their consumption of refined sugar, flour, and oils, which represent almost 60% of the calories consumed by the average American. Replacing these calories with vegetation (vegetables, fruits, nuts, and legumes) to achieve proper body weight can lead to a rapid normalization of CRP, glucose, triglycerides, and HDL cholesterol. Supplements that exert multiple anti-inflammatory benefits include fish oil, magnesium, and vitamin D. Vitamin C and zinc are also a good consideration as supplementation studies have demonstrated that participants developed fewer viral infections compared to those taking a placebo.
Consider the recommendations in the last two paragraphs... very straightforward and uncomplicated -we should all get healthy. To date, such recommendations have yet to be made by those in the media, government, or the medical profession in the context of battling COVID or viral infections in general, which is shameful. There is still time for the chiropractic profession to unify and deliver a consistent health-promoting message that the public needs to hear.
Dr. David Seaman became aware of the developing research that linked nutrition to the inflammatory process, while in clinical practice in the late 1980's, and noticed that appropriate dietary changes could significantly improve various musculoskeletal and visceral conditions. Based on this experience, he began to focus on nutritional approaches for inflammation/pain control and has followed the related scientific literature ever since. This led to the publication of the first book on nutrition for pain and inflammation, which was followed by many articles and book chapters devoted to this topic. His educational efforts resulted in being awarded the 2006 Academician of the Year by the American Chiropractic Association.
References
1. Seaman DR. Body mass index and musculoskeletal pain: is there a connection? Chiro Man Ther. 2013;21:15.
2. Seaman DR. The DeFlame Diet: DeFlame your diet, body and mind. Wilmington: Shadow Panther Press. 2016.
3. Seaman DF. The DeFlame Diet for Immune Health. Wilmington: Shadow Panther Press. 2020.
 View Full Issue
View Full Issue