Through my 40 plus years of experience, a patient with a herniated disc initially may make many different choices. Exercise, chiropractic care, and physical therapy may be helpful in some cases. However, when the front end of your car goes out of alignment, what happens to your tires? They wear. I have found some patients come down the road where all else has failed, leaving them with two essential choices:
1. Nonsurgical spinal decompression (NSSD)
2. Surgery
Now, when talking to Dr. Norman Shealy, who is not a fan of spinal surgery, he states that in extreme cases, it may be necessary. I agree. However, the earlier the issue is detected, the easier it’s corrected. A subluxation can become a bulge, and a bulge can become a herniation.
Dr. James Cox understood that and has done tremendous research on disc injuries. I recommend that every DC read his works because it will help in treatment. I originally started using much of Dr. Cox’s work. In my opinion, Dr. Dyer and Dr. Shealy took the treatment of disc injuries to the next level by adding technology and algorithms to expand basic traction. The Ramos and Martin study was pivotal in proving how nonsurgical spinal decompression can noninvasively help the disc and restore function.
Technology has changed the way we now can treat disc bulges and herniations. We live in a world driven by technology, and the consumer demands it. The perfect example is Apple and what they have done with phones and computers. My goal is that our profession takes the lead in the treatment of disc injuries and that surgery becomes the last option.
Predictability of Pain after Surgery
Some types of back surgery are far more predictable in terms of alleviating a patient’s symptoms than others. For instance:
•A discectomy (or microdiscectomy) for a lumbar disc herniation that is causing leg pain is a very predictable operation. However, a discectomy for a lumbar disc herniation that is causing lower back pain is far less likely to be successful.
•A spine fusion for spinal instability (e.g., spondylolisthesis) is a relatively predictable operation. However, fusion for multilevel lumbar degenerative disc disease is far less likely to be successful in reducing a patient’s pain after surgery.
Therefore, the best way for any patient to avoid spine surgery that leads to an unsuccessful result is to try nonsurgical spinal decompression first. Then give the patient time to heal and rehabilitate the core muscles.
Spinal decompression has been proven effective in relieving pain associated with bulging and herniated discs, degenerative disc disease, sciatica, and even relapse or failed back surgery. Since its release, clinical studies have revealed an amazing success rate in treating lumbar disc-related problems with spinal decompression.
Dr. Jason Kaplan, DC, explains it well. “Spinal Decompression uses state-of-the-art technology to apply a distraction force to relieve nerve compression often associated with low back pain and sciatica. You need to get spinal distraction without muscular contraction to succeed in obtaining the event called nonsurgical spinal decompression.”
In the past, many people thought that back pain was simply muscular in nature, I told the Bogduk study, Bogduk, N,: The Anatomical Basis for Spinal Pain Syndromes. JMPT 6:Nov.Decl995. There is no scientific basis for the belief that muscles are a source of chronic pain. However, controlled studies show how common disc and facet pain accounts for more than 70% of chronic back pain.
As we know, discs allow the spine to be flexible and let us lean forward or turn our upper body from side to side. Our discs also absorb shocks that are transferred to the spine while running, jumping, playing golf, etc.
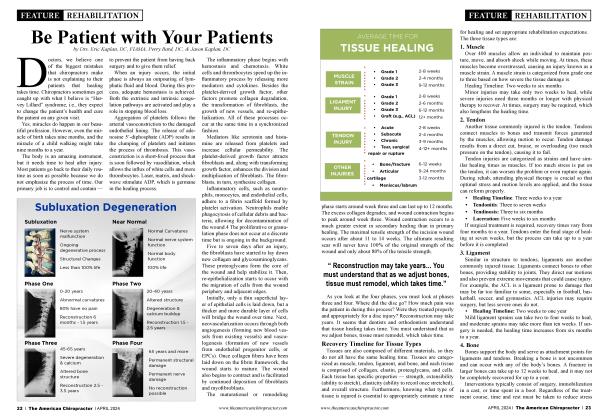
When you have a degenerated or bulging disc, one of the spinal discs is bulging beyond the edges of the vertebral bodies that are above and below it. There are three types of common terminology used to explain discs:
•Prolapsed disc - The disc is bulging between the vertebrae, but the disc’s outermost layer is still intact.
•Extruding disc - There is a tear in the outer layer of the spinal disc, causing the spinal disc tissue to leak out. However, the tissue that has come out remains connected to the disc.
•Sequestration - In this instance, spinal disc tissue has entered into the spinal canal and is no longer directly attached to the disc. It is the most serious type of slipped disc.
Inclusion Criteria:
•Pain due to herniated and bulging lumbar discs that is more than four weeks old.
•Recurrent pain from a failed back surgery that is more than six months old.
•Persistent pain from a degenerated disc not responding to four weeks of therapy.
•Patients available for four weeks of treatment protocol.
•Patient at least 18 years of age.
Exclusion Criteria: Contact the manufacturer for their exact exclusion criteria
•Appliances such as pedicle screws and rods
•Pregnancy
•Prior lumbar fusion less than six months old
•Metastatic cancer
•Severe osteoporosis
• Spondylolisthesis (unstable)
•Compression fracture of lumbar spine below LI (recent)
•Pars defect
•Pathologic aortic aneurysm.
•Pelvic or abdominal cancer
•Hemiplegia, paraplegia, or cognitive dysfunction
•Most patients do not experience any side effects, but there have been some mild cases of muscle spasm for a short period.
Decompression is achieved by using a specific combination of spinal positioning and varying the degree and intensity of force. The key to producing this decompression is the gentle pull created by an algorithm specific to your machine. No, all machines are not the same. When distractive forces are generated by specific software, the goal is for the typical proprioceptor response to be avoided. Avoiding this response allows decompression to occur at the targeted area.
Spinal decompression works to create a negative pressure or vacuum inside the disc. This effect causes the disc to pull in the herniation, and the increase in negative pressure also causes the flow of blood and nutrients back into the disc, allowing the body’s natural fibroblastic response to heal the injury and rehydrate the disc. Traction and inversion tables, at best, can lower the intradiscal pressure from a +90 to a +30 mmHg. Spinal decompression research by Ramos and Martin is shown to reduce the intradiscal pressure to between a -150 to -200 mmHg. Traction or inversion often triggers the body’s normal response to stretching by creating painful muscle spasms that worsen the pain in the affected area.
In the Journal of Neurological Research (1998), researchers stated, “We consider decompression therapy to be a primary treatment modality for low back pain associated with lumbar disc herniation at single or multiple levels, degenerative disc disease, facet arthropathy, and decreased spine mobility. Physiology (pain and mobility) and pathology correlate imprecisely. We believe that postsurgical patients with persistent pain or ‘failed back syndrome’ should not be considered candidates for further surgery until a reasonable trial of decompression has been tried.”
In the Journal of Neurological Research (2001), researchers stated, “For any given patient with low back and referred leg pain, we cannot predict with certainty which cause has assumed primacy. Therefore, surgery, by being directed at root decompression at the site of the herniation alone, may not be effective if secondary causes of pain have become predominant. Decompression therapy, however, addresses both primary and secondary causes of low back and referred leg pain. We thus submit that decompression therapy should be considered first, before the patient undergoes a surgical procedure, which permanently alters the anatomy and function of the affected lumbar spine segment.”
In that same volume of the Journal of Neurological Research, the senior lecturer in orthopedics at Sydney University stated, “Successful reduction of intradiscal pressures with decompression therapy represents a technological advance in lumbar spinal treatment and is likely to affect both the biomechanical and biochemical causes of discogenic pain.”
References
1.Mackenzie R: Mechanical diagnosis and therapy for disorders of the low back. In Taylor JR, TM’omeyLT (Eds.): Physical Therapy of the Low Back, Churchill Livingstone, New York, 2000p. 26 & 143.
2. Kushlich SD, Ulstrom RN, Michael CJ: Tissue origin of low back pain and sciatica. Orthop Clin North Am; (22): 181,1991.
3. Nachenson AL, Elfstrom G: Intravital dynamic pressure measurements of lumbar discs. Scand J Rehabil Med 2 Sitpp 1:1-40, 1970.
4. Yong, Hing K., Kirkaldy-Willis WH: Pathophysiology of degenerated discs of the lumbar spine. Phi la. The Ortho Clinics ofN. Am. Volf 14) #3 July 83, p.p. 493504.
5. BogdukN., Twomey L: Clinical Anatomy of the Lumbar Spine. Churchill Livingstone New York, 1992. p.p. 6869 & 151-173
6. Twomey LT: Sustained lumbar traction: an experimental study of long spine segments. Spine 1985; (10): 146-149.
7. Judkovich BD: Lumbar traction therapy: elimination of physicalfactors that prevent stretch. JAMA 1955; 159. 8.
8. Gose E, Naguszewski L: Vertebral axial decompression therapy: an outcome study. Neuro Research. (20)43, April 1998.
9. Mathews JA: Dynamic discography: a study of lumbar traction. Annals ofPhy Med, IX (7) 1968, p.p. 265-279. 10.
10. Colachis SC et al,: Effects of intermittent traction on vertebral separation. Arch of Phy Med & Rehab 1972 (50), p.p. 251-258.
11. Shealy CN. Borgmeyer V: Decompression, reduction, stabilization of the lumbar spine: a cost-effective treatmentfor lumbosacral pain. AJPM 1997; 7(2), 663 -665.
12. Winkle D et al,: Diagnosis and Treatment of the Lumbar Spine. Aspen: Maryland: 1996p.p. 303-313.
13. Degenerative disorders of the spine. In: Hochschuler SH, Cother HB, (Eds.) Rehab of the Spine. Mosby MO. 1993 p.p. 464-465 & p.260.
14. Cyriax JH: Illustrated Manual of Orthopaedic Med, London, Butterworths, 1983 p.p. 30-40.
15. Schiotz E, Cyriax JH: Manipulation: Past and Present, London, Heinemann, 1975.
16. Biomechanics. In: Hochschuler SH, Cother HB, (Eds.) Rehab of the Spine. Mosby MO. 1993 p.p. 146.
17. Kushlich S: Tissue origin of mechanical low back pain and sciatica. In: Hochschuler SH, Cotier HB, (Eds.) Rehab of the Spine. Mosby, MO. 1993, p.p.595-599.
18. Natural history of the lumbar spine. In Taylor JR, Twomey LT, (Eds): Physical Therapy of the Low Back, Churchill Livingstone, New York, 2000, p.p. 25-26 & 43-51.
19. Onel D et al,: Computed tomographic investigation of the effects of traction on lumbar disc herniations. Spine 1989; 14(l):82-9.
During 32 years as business partners, Dr. Eric Kaplan and Dr. Perry Bard have developed Disc Centers of America, Concierge Coaches, and the first national certification program for nonsurgical spinal decompression.
Dr. Jason Kaplan is a Parker University graduate practicing in Wellington, Florida with his wife, Dr. Stephanie Kaplan. Jason also is an Instructor for Disc Centers of America and teaches technique for the National Certification Program at Life University.
To learn more, visit thechiroevent.com or decompressioncertified.org, or call 888-990-9660.
 View Full Issue
View Full Issue