Do you remember the radio broadcaster, Paul Harvey? He was renowned for telling you a news story and then filling in the facts and stories that went on behind the scenes. He would always say, “And now... the rest of the story.” Listeners were in for a treat with what followed.
I have found that my patients are now giving me “the rest of the story” when presenting their report of findings. It is extremely gratifying to see patients have a “light bulb” moment while we review their report of findings. Their eyes get big, their brows raise, and they smile when it dawns on them that the chiropractor has hit on something they never thought of, and now they can make sense of the reason they have the pain that brought them in for care.
Beyond that, when you have done your examinations well and give patients your report of findings, they will start to provide information that they did not share during the initial patient history. Aches, pain, conditions that the patient never thought to be relevant come rolling out when they understand the biomechanics that only a chiropractor looks for and explains.
The Structural Fingerprint Exam®: Why it’s essential
Several years ago, I started utilizing the Structural Fingerprint Exam® protocols in my office. This was a huge benefit to me in my practice because it brought a systematic approach to my patient examination procedures. In my opinion, it took me back to the roots of chiropractic — looking at the structure and the biomechanics for the cause of disease. It also separated me from other providers the patient may have already seen who just listened to their chief complaint and did not consider the patient as a whole being.
The Structural Fingerprint Exam® consists of three components — ortho/neuro exam, X-ray imaging, and 3D digital foot scan. This article won’t delve into the details of each of these components. Instead, it will demonstrate how presenting the results of these three examinations can open the patient up to presenting “the rest of the story” that they did not initially tell you, which in turn opens the door for you to help them in ways they never imagined.
A patient case study: Going beyond the initial exam
Consider the following uncomplicated patient case. Marcia, age 34, presented to the office complaining of lower back pain with radiating left leg pain to the knee and occasionally to the lateral ankle and foot. The episode had begun three days earlier with acute pain that she rated at 7/10 and described as severe. She began working out at home about four months ago. She had several mild episodes of lower back pain and stiffness during that time, but nothing caused her to restrict or limit her activities until the most recent onset three days earlier.
 Figure 1
Figure 1
Her physical exam revealed moderate loss of active range of motion on lumbar extension with pain. Her lumber flexion was mildly restricted with pain, and her left rotation was mildly restricted. The ortho/neuro exam was rather unremarkable with lower extremity reflexes 2/2 and lower extremity strengths 5/5. The only positive tests were Nachlas on the left and Yeoman’s bilaterally. On visual exam, pronation was noted in the feet bilaterally with an altered Q angle on the left.
Marcia’s case was setting up to be a classic facet syndrome of the lower lumbar spine on the left, which it was. However, by proceeding with X-rays and a 3D digital foot scan, we uncovered other biomechanical faults that gave the patient that light bulb moment and the opportunity for me to hear the rest of the story. Now let us consider the biomechanical findings noted on X-ray and 3D digital foot scan. The lumbar AP (Figure 1) revealed a lower femoral head on the left and a left towering of the lumbar spine. The lateral lumbar (Figure 2) demonstrated an anterior Ferguson’s line (or an anterior lumbar gravity line) and a sacral base angle that measures 44 degrees.
The 3D foot scan showed moderate pronation, with the left medial longitudinal arch being pronated more than the right. There also was more weight distribution on the left compared to the right.
So here is a summary of the findings:
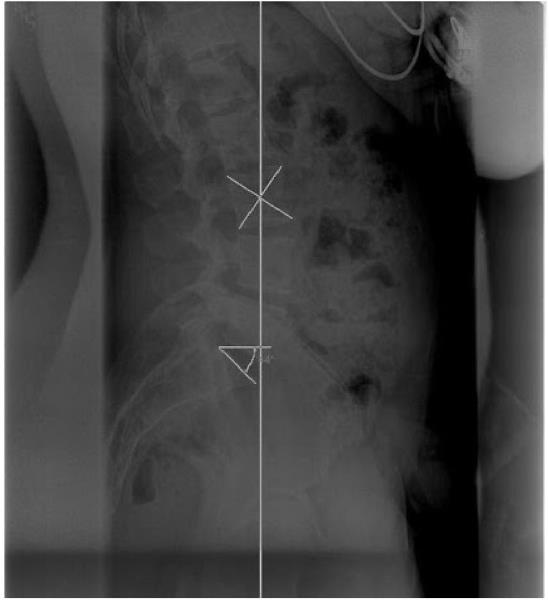 Figure 2
Figure 2
Now the rest of the story ...
If I had stopped with just the ortho/neuro exam, the correct diagnosis would still have been rendered — facet syndrome of the lumbar spine. A course of spinal manipulative therapy would have been undertaken with appropriate modalities, and the patient would have responded well.
However, when presenting the report of findings to the patient, she had a light bulb moment and told me the rest of the story. It started out in the form of a question. “I have been wearing braces on both of my knees when I run, but my left knee has been hurting more. Could that have been caused by these things you have told me?” Then, she added the follow-up question, “I have had plantar fasciitis off and on for three years. Could the fallen arches and unlevel hips have caused that?”
BINGO! The rest of the story. Marcia had other musculoskeletal complaints going on that she did not reveal during the initial patient interview. Those conditions had a biomechanical origin related to her chief complaint. They never would have been revealed to me if the biomechanical information had not been discovered through X-ray and foot scan analysis combined with the ortho/neuro exam.
Marcia’s is not the only case. In fact, it is the norm rather than the exception, and it reinforced two key concepts:
If the examination had stopped with ortho/neuro, the rest of the story might never have been told.
Your report of findings can provide the patient with an understanding of their complaint and open the door for additional treatments and services that will help you care for the patient more completely. As I say in my seminars, “Don’t chase the symptoms; solve the biomechanical problem.” When you perform a thorough biomechanical assessment, you allow the patient to discover how much more you can do for them. In a world where people are dying by the tens of thousands from opioid abuse, chiropractic needs to stand in the gap. We have the tools, skills, and education to provide better assessments and better treatments. Chiropractors need to set themselves apart from other providers by being the biomechanical experts who can handle the musculoskeletal epidemic. When we do what others are not doing and act as the biomechanical experts upon which chiropractic was founded, then our patients will reveal. . . the rest of the story!
Dr. Jeff McKinley received his bachelor's degree in biology from Lipscomb University in Nashville, Tennessee, and his doctorate from Logan College of Chiropractic. He completed postdoctorate training in sports injuries and is a certified chiropractic sports physician (CCSP). He has been part of the Pioneer Sports Medicine Team at Warren County High School for over 25 years, working with the athletic trainer, orthopedic surgeon, physical therapist, and EMT to care for high school athletes.
 View Full Issue
View Full Issue