A novel nondrug approach to the prevention of menstrual migraine
November 1 2022 Eric LieblerA novel nondrug approach to the prevention of menstrual migraine
November 1 2022 Eric LieblerFor the over 28 million American women who experience a migraine each year, one of the most common migraine triggers is something that they can’t avoid — their monthly menstrual cycle. A menstrual migraine (MM) or hormone headache starts before or during a woman’s period and can happen every month. Common symptoms include a dull throbbing or severe pulsing headache, sensitivity to light, nausea, fatigue, dizziness, and more. Unfortunately, the migraines can also occur outside of the direct menstrual cycle in what is called a menstrually related migraine (MRM). Many ask if this “hormone-driven” migraine is different from a migraine triggered by something else. While there isn’t a clear-cut answer, the literature often suggests that menstrual migraine can tend to be more severe, last longer, and be less responsive to treatment than other types of migraine.
This presents providers and their patients with a challenge. There is an identifiable trigger, and you know when the trigger is coming, but what treatment options are available? A host of pharmacologic (drug) options have been studied and approved for the prevention of migraine over the past several years. Historically, some drugs being utilized were originally developed as anti-seizure medications, such as divalproex sodium and carbamazepine. In addition, several new injectable monoclonal antibodies and oral drugs that target calcitonin gene-related proteins (CGRP) have been approved for migraine prevention but have not yet been studied specifically in menstrual migraine. These treatments may not be ideal for many women who wish to avoid long-term daily treatment for migraine attacks that typically occur within a well-defined time frame. Many women may also prefer a treatment that does not come with any of the potential side effects that could occur with long-term drug treatment.
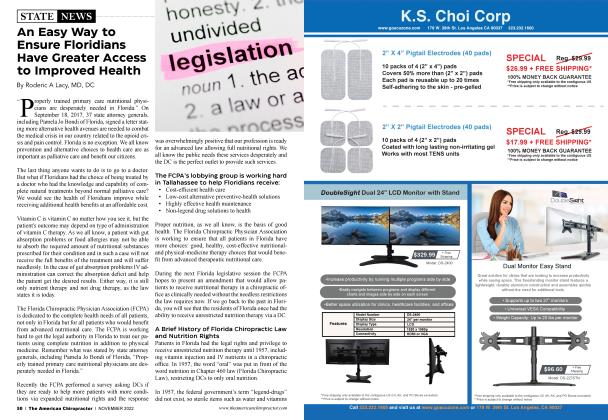
In these cases, neuromodulation through a convenient, noninvasive treatment may be ideal for many patients. Noninvasive vagus nerve stimulation (nVNS) has been studied as both an acute and preventive treatment for menstrual and menstrually related migraines. In a controlled study of nVNS in women with menstrual migraines, where the women only used nVNS around the time of their menses, the number of attacks per month as well as the use of other medications significantly decreased with nVNS — from 7.2 attacks per month to 4.7 (p0.001) while the decrease in medication use per month went from 8.9 times per month to 5.6 (p0.001).
Change in the Number of MM/MRM Days per Month (ITT population)
From Grazzi L, Egeo G, Calhoun AH, McClure CK, Liebler E, Barbanti P. Non-invasive vagus nerve stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migrane: an open-label study. J Headache Pain. 2016;17(1):91. doi:10.1186/s1094-016-0684-z
The authors concluded by noting, “This study suggests that mini-prophylaxis with nVNS is an effective treatment that reduces the number of menstrual and menstrually related migraine days and acute analgesic use for subjects with MM/MRM without adding any treatment-related safety or tolerability concerns. The current study also expands the body of evidence regarding this condition. As the first neuromodulation technique evaluated in patients with MM/MRM, nVNS may offer an important new option for effectively treating the condition while mitigating the monthly perimenstrual AE [adverse event] burden and potential complications of pharmacologic medications.”
nVNS offers great flexibility for the chiropractic community as a nondrug option that can be integrated into a chiropractor’s migraine toolbox, providing the option to further enhance your ability to manage your patient’s overall health without the need for headache specialist referrals. In addition to being approved for the acute prevention of migraine and cluster headache, nVNS is also currently being investigated in a range of areas of interest to the chiropractic community, including post-traumatic stress disorder (PTSD) and nausea for those suffering from gastroparesis.
Eric Liebler has 30+ years of neurological experience. He currently leads clinical trial research at electroCore and supports the scientific and medical affairs efforts. Eric is an author of more than 50 papers focused on the clinical use of nVNS. In 2009, he co-founded Nautilus Neurosciences, a neurology-focused specialty pharmaceutical company focused on identifying and developing drugs benefiting those affected by neurological disorders and brought to market Cambia® (diclofenac potassium) for the treatment of acute migraine. He can be contacted at [email protected].
References
1. Moy G, Gupta V. Menstr ual Related Headache. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https:/Avww. ncbi. nlm. nih.gov/books/NBK55 7451/
2. Rashid A, Manghi A. Calcitonin Gene-Related Peptide Receptor. [Updated 2021 Jul 17]. In: StatP earls [Internet]. Treasure Island (FT): StatP earls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b...
3. Grazzi L, Egeo G, Calhoun AH, McClure CK Liebler E, Barbanti P. Non-invasive vagus nerve stimulation (nVNS) as mini-prophylaxis for menstrual menstrually related migraine: an open-label study. JHeadache Pain. 2016; 17(1):91. doi: 10.1186/si 094-016-0684-z
 View Full Issue
View Full Issue