Smart Healing Takes Time
REGENERATION
Eric Kaplan
DC, FIAMA
Perry Band
DC,
Jason Kaplan
DC
During 34-plus years as businesspartners, Dr. Eric Kaplan and Dr. Perry Bard have developed Disc Centers of America, Concierge Coaches, and the first national certification program for non-surgical spinal decompression a 12 CEU credit event. Being held for the 10th anniversary on November 5,6. This event has been sold out for two years running. Dr. Jason Kaplan is a Parker University graduate practicing in Wellington, Floridawith his wife, Dr. Stephanie Kaplan. Jason also is an Instructor for Disc Centers of America and teaches techniques for the National Certification Program at Life University. To learn more, call 888-990-9660 visit thechiroevent.com or decompressioncertified.org.
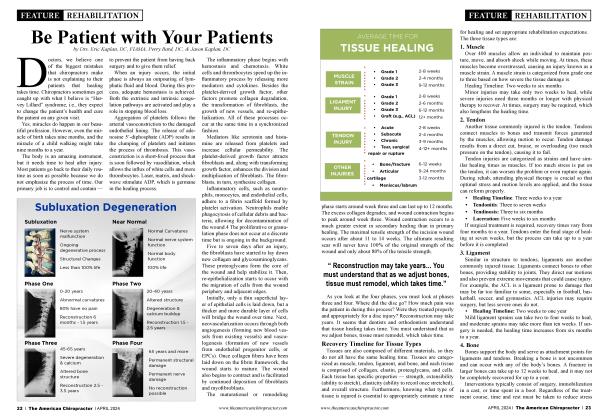
Approximate Rate of Tissue Healing
Too many doctors have unrealistic expectations about healing. Dr. Bard and I continually look for research to educate our patients. We talked about this at Bootcamp and will be going into more detail at the National Certification event in October. Are you enrolled yet? It is a Life University-sponsored event offering 12 CEUs.
Just like Rome, the human body wasn’t built in a day, and it certainly won’t repair itself in that time. After your treatment plan, healing still takes place, and scar tissue must fonn to secure the vertebrae because you’ve been pulling on them for 20 to 30 visits. Symptoms will improve, but expecting all of them to be asymptomatic is not realistic.
The body’s response to damage is complex and variable, depending on the extent of damage, the type of tissue, age, health, and many more uncontrollable variables, especially when it comes to discs. You cannot control how fast a patient’s body repairs itself following injury. You can only optimize it by avoiding factors that slow the normal healing process. Even during decompression, discs are active and probably overdoing it.
Patients must avoid activities that reinjure the tissue, such as lifting for a disc injury, golfing, etc. For example, running after a hamstring strain or even standing on a fractured foot is not recommended.
Activity that reproduces your pain and makes it more sensitive or intense is likely limiting the ability to heal, so “no pain, no gain” is not a recommended mindset. With decompression, be mindful and patient not to overpull and reduce the weight and time of the pull. Just like how the body deals with a cold or infection, it has a process to deal with tissue damage. Tissue describes a collection of similar body cells, such as muscle, epithelial, connective, and nerve. The healing process is similar for each tissue type, with small variations in the cells involved.
Not every tissue type will heal in the exact same manner because of the blood supply to the area, the function of the tissue, and the ability to protect the tissue in response to injury. The majority of tissue injuries occur when a large amount of pressure is placed on a structure. The pressure, whether quickly applied or accumulative over time, causes the breakdown of tissue and damage occurs.
An immediate reaction begins in response to tissue damage, which occurs in four distinct phases. Each phase takes time to complete, and they usually overlap before the next one begins. At Disc Centers of America, we continually educate the patient. Here is a chart you can utilize with your patient education:
Phase One: Bleeding
Bleeding is the vascular component of inflammation. The immediate response to damaged tissue is usually bleeding and swelling around the injured tissue. With low back and neck injury, trauma is usually associated.
Trauma occurs at a cellular level when cells and blood vessels that make up the damaged tissue die and release a chemical called histamine, which increases the rate of fluid flooding the area from the surrounding blood vessels. That causes dilation of blood vessels surrounding the damaged tissue, allowing migration of white blood cells, platelets, and other blood products in and around the damaged tissue, starting the cellular inflammatory process. This occurs immediately following tissue damage and is managed in minutes to hours after injury.
Phase Two: Cellular Inflammation Phase
The arrival of blood products to the damaged site allows the tissue to prepare for the healing process. White blood cells, specifically leukocytes, infiltrate the damaged tissue and consume debris and dead tissue in a process called phagocytosis.
Once the damaged tissue is removed, the remaining tissue is prepared for rebuilding, and the damaged cells no longer produce inflammatory chemicals, slowing down the inflammatory process. When damaged tissue is unable to be completely cleared or removed from the damaged site, inflammation continues to cycle without stopping, which is chronic inflammation.
The normal process of inflammation spans between minutes following initial damage and the next 72 hours after the injury.
Phase Three: Proliferation
In the dying stages of inflammation, specialized cells called fibroblasts begin to rapidly multiply in and around the damaged tissue in a process called proliferation. Fibroblasts reconstruct damaged blood vessels in the area and lay down bundles of collagen to rebuild the damaged tissue at the injury site, which may include surrounding muscle/connective/ epithelial tissues also damaged by the abnormal load, causing tissue breakdown.
Once the immature tissue is laid down, the wound begins to contract to reduce the size of the damaged site. Laser therapy helps expedite healing, which is why Disc Centers of America doctors like using it.
This phase begins on the first day of injury and extends up to a month after it.
Phase Four: Remodeling
Remodeling describes the maturation of immature collagen cells within the wound that are roughly laid out in the proliferation phase.
Type III collagen, which is laid down in the proliferation phase, is disorganized and randomly orientated. It converts during the healing process to type I when gentle force is applied, such as stretch, contraction, or weight-bearing pressure to the healing tissue. That aligns the fibers with the direction of tension and reduces the occurrence of scar tissue.
This process begins in the weeks following tissue damage and can extend over 12 months or more, depending on the size and type of the injury or wound.
There are five components of a subluxation:
1. Kinesiopathology
2. Neuropathology
3. Myopathology
4. Histopathology
5. Pathophysiology.
Let’s Talk Disc
Stages One and Two: Disc Protrusion and Prolapsed Disc
The first two stages of disc herniation (disc protrusion and prolapsed disc) are incomplete herniations. During these two stages, the gel-like substance called the nucleus hasn’t yet leaked through the outer layer. Instead, the nucleus puts pressure on the outer tissues and causes the disc to protrude.
Stage one often doesn’t present any symptoms because the protrusion isn’t signihcant enough to put pressure on the nearby nerves.
Once the protrusion reaches the second stage, the patient may feel pain in the area where the prolapsed disc is located. This is why an MRI is so important during treatment.
Stages Three and Four: Disc Extrusion and Sequestration
During the third and fourth stages of disc herniation (disc extrusion and sequestration), the nucleus breaks through the wall of the disc, and healing will take longer as more tissue is involved.
In the final stage, not only does the nucleus leak out, but it also begins dripping out of the disc. Leg drop and incontinence may be symptoms, again confirmed by an MRI.
Why do some herniated discs take so long to heal? They have a poor natural blood supply. Remember, we are dealing with the five components of subluxation, and each segment must heal in its own time.
We have found often the better the equipment, the more updated the technology; the better the result. NSSD, with IDD, is endorsed by Neurosurgeon & former Harvard Medical School professor, Dr. Norman Shealy M.D., PhD, for it helps create imbibition, which provides nutrients and fluid to the disc. Dr. Shealy also endorses DCOA, Disc Centers of America, now in 43 States and Canada.
Blood how is the means of both providing nutrients to an injured structure and clearing away debris. The discs do not have a direct blood vessel to them, so blood must diffuse through the bones (vertebrae) to reach the disc and diffuse out once it has done its job. This takes a lot longer than when blood is delivered directly through a vessel to its target structure, and that’s why proper hydration, supplements (including omega-3 fatty acids), and proper exercises are an import ant part of the healing process.
This is also why improving blood how using laser therapy is key to improving recovery horn a herniated disc and can cut the time it takes to heal.
 View Full Issue
View Full Issue