During the COVID hiatus, Dr. Tim Maggs analyzed data he collected in his office over the prior three-and-a-half-year period regarding leg length. With more time than normal because of COVID, Dr. Maggs proceeded to have three research papers published in a medical peer-reviewed journal (available on DrTimMaggs.com). The first study gave the details of 351 patients who had a standing A-P L-S X-ray taken while barefoot. The femoral head height difference (FHHD) was measured and documented. Each patient also had their feet digitally laser-scanned, and after they purchased custom orthotics, the orthotics were inserted into their shoes, and a second standing A-P L-S X-ray was taken. The FHHD was measured again and documented.
The second paper looked at the same 351 patients to see how many had FHHD greater than 3 mm and greater than 5 mm both while barefoot and then with orthotics. The purpose of this study was to see how custom orthotics affects FHHD.
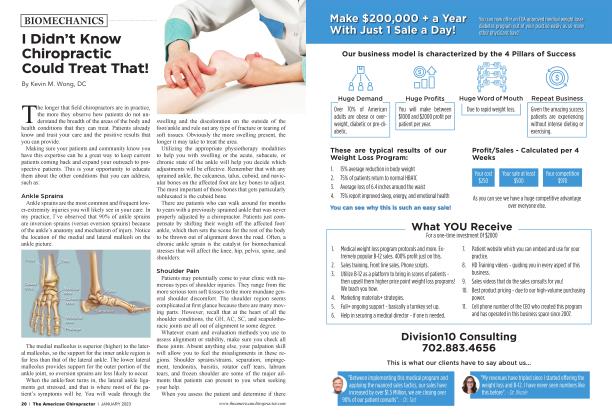
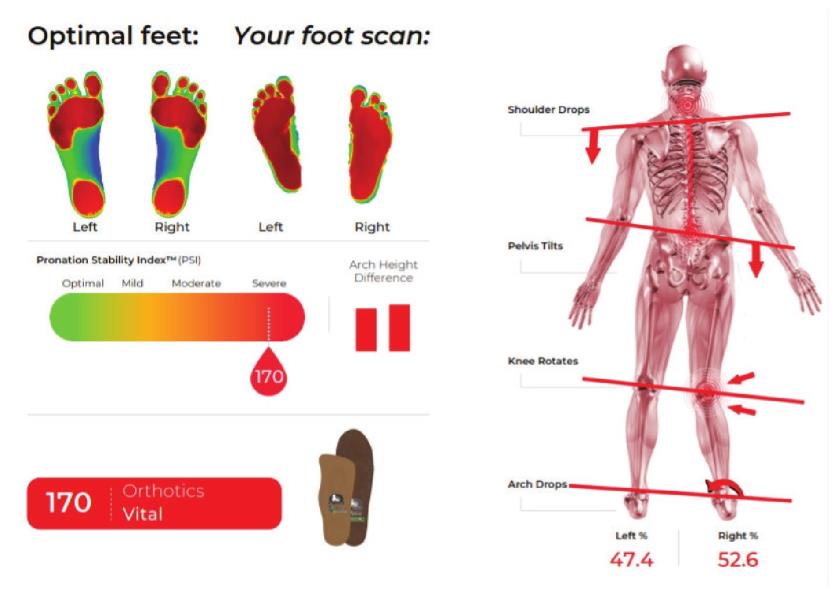 Figure 1
Figure 1
The third paper studied 400 patient foot scans (fig. 1) and collected relevant data to determine how many people have collapsed arches and if arches continue collapsing over one’s lifetime. According to Dr. Maggs, these findings should change the way all of us evaluate patients. All chiropractic techniques are limited in their benefits because FHHD due to foot collapse and leg length difference affects every human, but virtually no one includes this testing in the initial patient evaluation. Chiropractors pride themselves on detecting and correcting subluxations, but any “correction” is merely temporary. The abnormal loading seen in these three studies is the primary contributor to subluxations, but these imbalances are never detected or corrected. The Maggs Leg Length Test should become a standard procedure before any treatment is recommended.
TAC: After almost 40 years of practice, what inspired you to enter the research world?
TJM: I never knew that giving a patient custom orthotics could possibly make their femoral head height difference (FHHD) worse. It happened in November 2017. After months of this young soccer player complaining of right apophysitis pain after giving him orthotics, I retook his X-ray with his orthotics in the shoes, and his FHHD went from 4.3 mm while barefoot to 6.0 mm with orthotics. To add insult to injury, he also had a stress fracture. My procedures changed that day. I proceeded to collect data on 351 patients over the next three years. I then analyzed the data. What I learned should forever change the guidelines of musculoskeletal testing for every patient, whether symptomatic or not.
TAC: What were your procedures prior to this patient?
TJM: I’ve used the biomechanical model for the past 30 years. I would perform a digital laser foot scan with two low-back and two cervical X-rays with the patient barefoot. When appropriate, we’d order orthotics for the patient, put them in their shoes, and begin treatment.
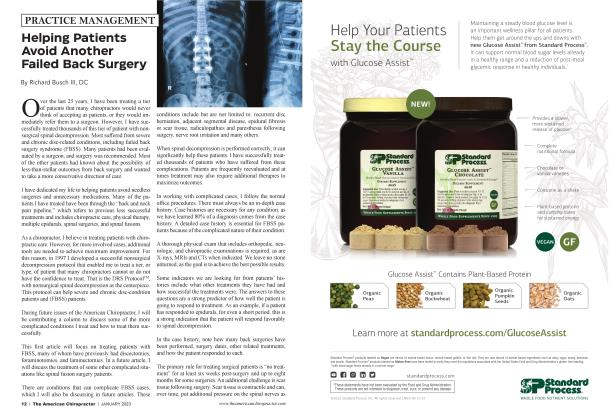
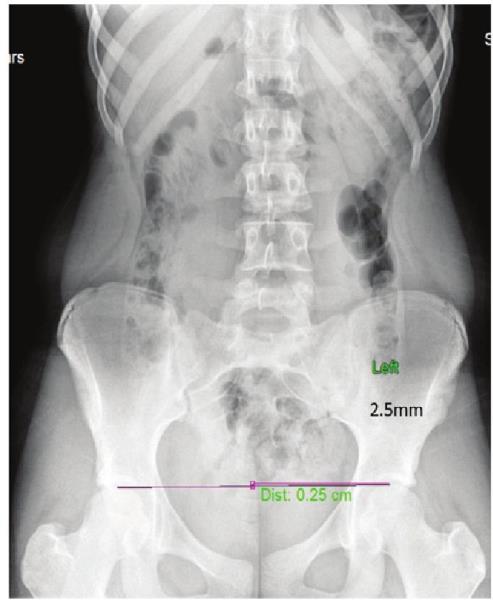 Figure 2
Figure 2
TAC: And your new procedure?
TJM: We continue the same procedure; we just added a standing A-P L-S X-ray with shoes and orthotics on (fig. 2). That gave us two numbers to work with. I believe this is the first time a study of this size has been done on this topic. Logan College began a similar study in 2002, but they used the iliac crests as reference points, only looked at 35 patients, and stopped the study prematurely because of findings they didn’t know what to do with.
TAC: What were your findings?
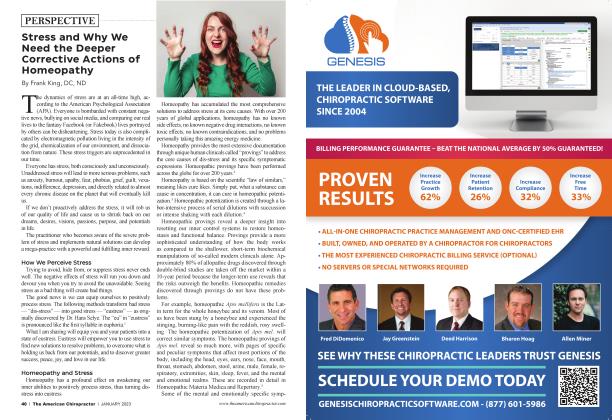
TJM: Before I started the study, I thought if a person’s FHHD was unlevel, once you put orthotics in the shoes, the FHHD would improve. I think that’s the general belief within the industry too. We learned that’s not true. We learned that some get better, some get worse, and some stay the same. We also learned that some start imbalanced (> 3 mm difference) and some start at what appears to be balanced (3 mm difference), but these measurements are not the patient’s true FHHD. Overall, we learned there are five different biomechanical patterns (Fig. 3) that are possible, and every human falls into one of the five categories.
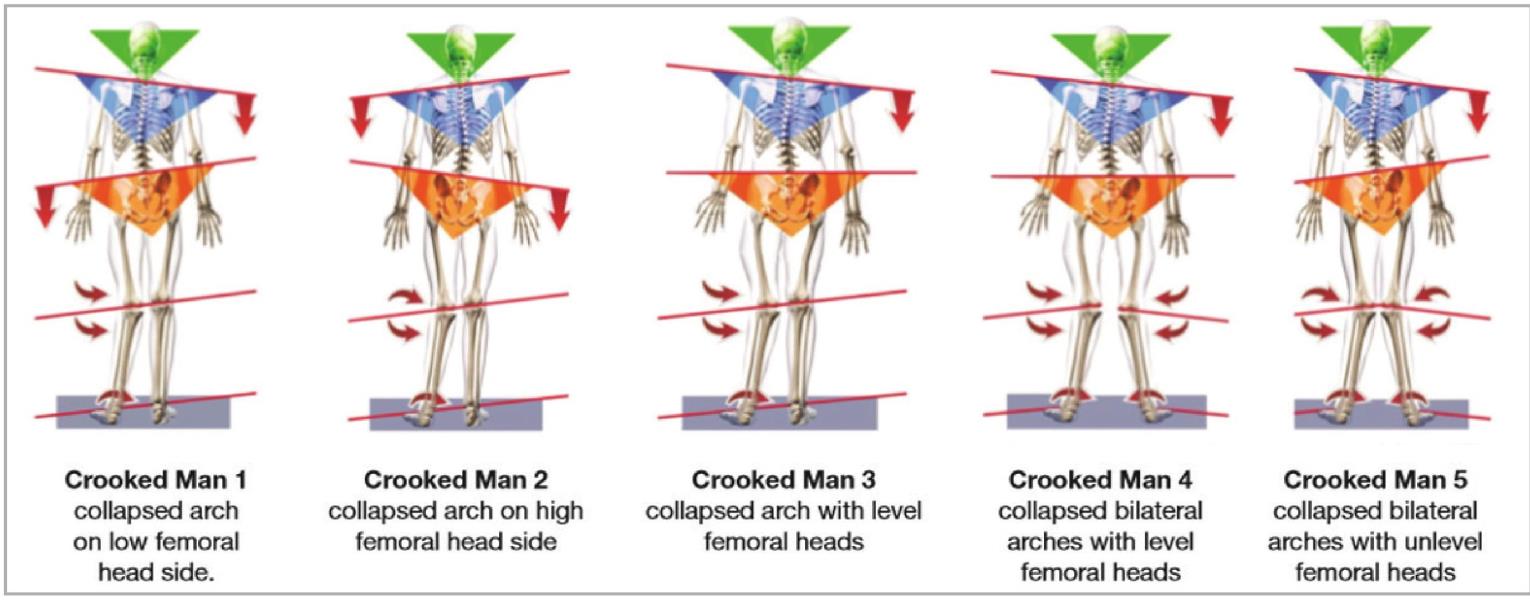 Figure 3
Figure 3
TAC: What is the Maggs Leg Length Test? TJM: First of all, I named this test to ensure it would not be confused with any of the other leg-length tests that exist out there. There are many. Some measure from the greater trochanter to the lateral malleolus with the patient prone. There’s the Deerfield Test. There’s the scanogram, and I’m sure there are many others. I developed this test because it’s the only test done in the standing position that takes into consideration both the collapse of the feet and the difference in actual leg length. It also uses today’s most advanced technology.
TAC: How do the feet play a part in a patient’s FHHD?
TJ M: Our third published paper reported on 400 patients we scanned using Foot Leveler’s digital laser scanner. It measures multiple factors, but primarily, it gives you a pronation index, which is the amount of collapse in each foot. It gives you the amount of space under each foot, and it gives you the percentage of body weight, right side versus left. After 400 scans, we learned two important findings; every patient has mild to severe collapse of one or more arches of the feet, and secondly, feet continue to collapse over the course of one’s lifetime. In addition, the feet do not collapse evenly in most cases. There is more weight-bearing on one side, which makes that foot collapse more. So if you are truly concerned with leveling the femoral heads, which I think is of paramount importance, then the patient should be fitted with custom orthotics and have a second standing A-P L-S X-ray to determine the new FHHD. With that information, appropriate corrections can be made.
Crooked Man 1-Barefoot - > 3 mm
Crooked Man 2-Barefoot - > 3 mm
Crooked Man 3-Barefoot - 3 mm
Crooked Man 4-Barefoot - 3 mm
Crooked Man 5-Barefoot - > 3 mm
With orthotics-improves by at least 1 mm.
With orthotics-the difference increases by at least 1 lmn.
With orthotics - > 3 mm difference.
With orthotics - 3 mm difference.
With orthotics - >3 lmn and less than 1 mm difference.
TAC: How common is FHHD?
TJM: FHHD is far more common than you think. And, measured with orthotics and without orthotics, there’s not much of a difference. Without orthotics, 64% are greater than 3 mm, and 42% are greater than 5 mm. With orthotics, 61% are greater than 3 mm and 40% are greater than 5 mm. To ignore these findings, knowing that musculoskeletal is the leading cost in health care makes no sense.
TAC: What are your conclusions after completing these studies?
TJM: I believe the chiropractic profession is the most qualified to examine, recommend, and treat the musculoskeletal system more than all other professions. I’m amazed that so many in our profession don’t X-ray. I’m amazed, after giving hundreds of seminars around the country, that so many chiropractors won’t recommend orthotics for varying reasons. Every human has biomechanical faults in their feet and leg lengths, but many ignore this fact when caring for patients.
I’m amazed that we, as a profession, are in the position to lead the industry in the prevention, diagnosis, and treatment of most musculoskeletal conditions, but we elect to imitate the medical model of care, the reactive model in the hopes of better reimbursement, and ignore the more advanced procedures that not only prevent but also predict future musculoskeletal breakdown.
My hopes are that our leading associations in the profession, the top companies who help support the profession and the schools, take a more conscientious look at our identity in the industry and have the courage to become leaders instead of followers. We are positioned to provide the highest level of care for the public, both diagnostically and therapeutically. Until we identify ourselves as leaders and begin practicing in such a manner, we’ll continue being an alternative with an identity the public doesn’t understand. A tremendous unifier for our profession would be to adopt the Maggs Leg Length Test as a universal test for all patient care.
Dr. Tim Maggs is a graduate of the National College of Chiropractic and has been in private practice for 44 years. He has specialized in the diagnosis and treatment of sports injuries throughout his entire career. He is the President of Dr. Tim Maggs Sports Chiropractic and Health Center in Schenectady, NY. He established the Concerned Parents of Young Athletes™ (CPOYA) Program. He partnered with Foot Levelers to develop their CPOYA custom orthotic and has lectured nationally for 20 years. In 2023 he will be introducing his Dr. Maggs Feet First System™. He can be reached at [email protected].
References
1. The Journal of Orthopedic and Rheumatology Open Access Journal
Catch this interview and many more TAC TIC Talks by scanning the QR code or visiting this link: tacadmin.qrd.by/TACTicTalk
 View Full Issue
View Full Issue