The New Age of Regenerative Medicine
October 1 2025 Sean Vandersluis, Dr. Adam BrockmanThe New Age of Regenerative Medicine
October 1 2025 Sean Vandersluis, Dr. Adam BrockmanMesenchymal Stem Cell Derived Extracellular Vesicles
“SASP factors activate immune cells and induce neighboring cells to also enter senescence, creating a self-perpetuating cycle of tissue dysfunction.”
Aging is the most significant risk factor for a wide array of chronic diseases, including respiratory diseases, neurological disorders (ND), cardiovascular disease (CVD), osteoarthritis (OA), and other metabolic disorders.1,6 Although these diseases have different physiological manifestations, they share a common origin — inflammation and cellular dysfunction.
Over time, intrinsic and extrinsic stressors drive genomic instability, mitochondrial inefficiency, and oxidative stress.6 Additionally, cells have a finite replicative lifespan. With each division, telomeres, the protective caps at the end of chromosomes, shorten. These changes push cells into senescence, a nondividing but metabolically active state characterized by the secretion of pro-inflammatory cytokines, chemokines, and proteases collectively termed the senescence-associated secretory phenotype (SASP).4
SASP factors activate immune cells and induce neighboring cells to also enter senescence, creating a self-perpetuating cycle of tissue dysfunction. This leads to chronic inflammation, or “inflammaging,”7 which disrupts tissue microenvironments, stem cell niches, and intercellular communication, ultimately impairing tissue repair and increasing disease susceptibility.
Reversing these changes requires regenerafive therapies that reduce inflammation, restore homeostasis, and reactivate intrinsic repair mechanisms. Such therapies offer promising potential for treating age-related diseases.2
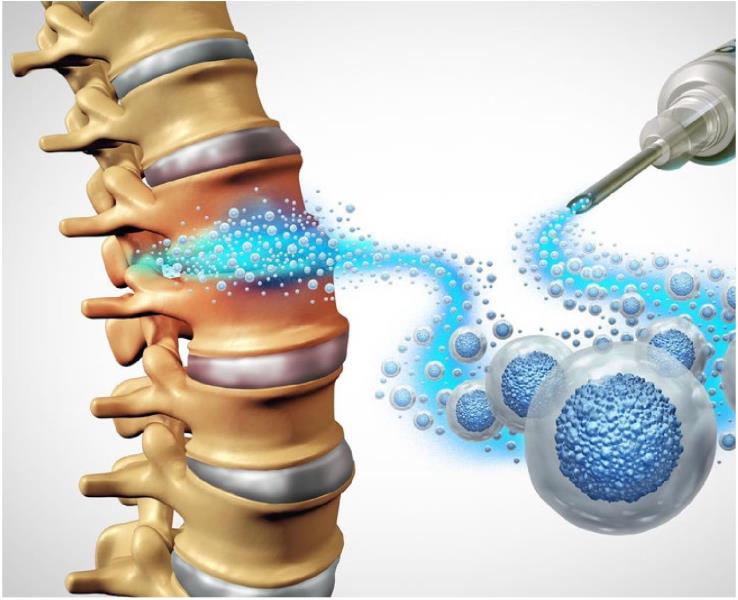
Mesenchymal Stem Cell Extracellular Vesicles: Cell-Free Regenerative Medicine
Mesenchymal stem cells (MSCs) have emerged as a promising tool in regenerafive medicine because of their unique ability to modulate immune responses, rejuvenate damaged cells, and promote tissue repair. Found in many tissues, including bone marrow (BM), adipose tissue (AT), and the umbilical cord (UC), MSCs are multipotent cells capable of self-renewal and differentiation into osteoblasts, chondrocytes, and adipocytes.3
Their biological role involves sensing tissue injury, migrating to the site, modulating immune activity, and releasing molecular signals that guide stem and progenitor cells in tissue regeneration.5 MSCs have garnered substantial research interest as regenerative medicine therapeutics because of their unique biological function. Indeed, MSC-based therapies have shown promise in preclinical and early clinical studies across many diseases over the past 15 years.8
Limitations of Cell-Based Therapies
However, several limitations hinder broader adoption.9 Systemic administration via intravenous infusion often results in MSC accumulation in the lungs, liver, and spleen, reducing availability at target tissues.10,11 This is particularly problematic for treating diseases of the central nervous system (CNS), where MSCs cannot efficiently cross the blood-brain-barrier,12 further restricting effective doses.
Direct delivery methods (e.g., intracerebral injection) improve targeting12,13 but can be invasive and are not feasible for every patient. Immunogenicity is another concern. Although MSCs express low levels of HLA antigens, allogenic rejection can still occur, and their proliferative capacity poses a tumorigenic risk,14 limiting repeat dosing.15
Paradigm Shift to MSC-EV Therapies
Mounting evidence suggests that much of MSC’s therapeutic benefit is mediated by extracellular vesicles (EVs), which are nanoscale, membrane-bound packages containing bioactive cargo, such as growth factors, cytokines, lipids, mRNA, and microRNAs, to target cells.6 MSC-derived EVs offer a cell-free alternative that addresses these limitations.
EVs are generally classified into three main subtypes — exosomes (30150 nm), microvesicles (100-1,000 nm), and apoptotic bodies (500-2,000 nm) — with exosomes being the most abundant subtype secreted by MSCs. Their small size allows them to circulate systemically with less accumulation in off-target tissues, and they can effectively cross the blood-brain-barrier enabling noninvasive delivery to the CNS.16 Like cells, EVs are composed of a lipid bilayer but contain lower levels of HLA markers and have no replicative capacity, rendering them even less immunogenic and tumorigenic, which facilitates repeat dosing.17
From a manufacturing standpoint, EVs are much easier stored long term, allowing for off-the-shelf therapies. These benefits position MSC-EVs as a safer and more clinically versatile therapeutic while retaining the immunomodulatory and regenerative signaling capacities that make MSC therapies effective.
Mechanisms of MSC-EV Regeneration Preventing Further Damage: Immunomodulation
Immunomodulation is a primary mechanism by which MSC-EVs exert their regenerative effects.18 MSCs detect inflammatory cues in the tissue microenvironment through pattern recognition receptors, including toll-like receptors, and respond by secreting EVs enriched with anti-inflammatory molecules, including prostaglandin E2 and interleukin-10.2 This cocktail suppresses SASP cytokines like TNTa and IL-6 by targeting pathways including NF-KB, JAK/STAT, and MAPK/ERK.2-6
Macrophages are reprogrammed from a pro-inflammatory Ml to an anti-inflammatory M2 phenotype,19-20,21 while dendritic cell maturation is inhibited, reducing T-cell-mediated responses and shifting the microenvironment toward an anti-inflammatory state.22
SASP cytokines also drive extracellular matrix (ECM) remodelling and fibrosis in conditions like OA.23 MSCEVs counteract this by reducing levels of tissue-degrading enzymes like matrix metalloproteinase-1 (MMP1),24 downregulating fibrosis-associated proteins like a-smooth muscle actin25 and upregulating ECM structural components like collagen type II,26 ultimately restoring tissue integrity. By reprogramming the immune enviromnent, MSCs support a regenerative state, limiting further damage from activated immune cells.
Rejuvenating Senescent Cells: Activating Regenerative Signaling and Survival Pathways
Beyond inflammation control and ECM remodelling, MSC-EVs actively promote tissue repair by rejuvenating senescent cells and activating stem/ progenitor repair pathways. MSC-EVs activate mTOR signalling to enhance cell proliferation and ERK signalling to promote cell migration toward injury sites.2-6 They promote cell survival by upregulating anti-apoptotic genes like BCL227 and downregulating pyroptosis regulators, including caspase-1.28
Oxidative stress and mitochondrial dysfunction are reduced via EV-mediated delivery of antioxidant enzymes, functional mitochondria, and induction of endogenous antioxidant pathways.29 These changes reduce SASP secretion, synergizing with the immunomodulatory effects. Once rejuvenated cells exit senescence, MSC-EVs activate tissue-specific repair pathways in stem/ progenitor populations to allow tissue regeneration.
Therapeutic Potential of MSC-EVs
These molecular effects translate into the tangible therapeutic outcomes observed across a variety of conditions. While clinical studies on MSCEVs remain limited — primarily in COVID-1930,31 — they are expanding as preclinical data continues to show efficacy in OA, respiratory diseases,2 ND,32 and CVD, amongst others.
The treatment of OA with MSC-EVs is currently the most well studied. OA progression is driven in part by pro-inflammatory Ml macrophage in synovial tissue.33 MSC-EVs have been shown in preclinical studies to promote M2 macrophage polarization, reduce synovial inflammation, and stimulate chondrocyte-driven ECM formation via ERK, AKT, and Wnt5a signaling.19 21
Intra-articular injection in animal models preserved cartilage thickness and reduced joint degeneration,34 and a recent clinical trial in patients with knee OA reported significant improvements in both pain and functional outcomes following MSC-EV injection.35 During the COVID-19 pandemic, a phase 1 clinical trial involving intravenous MSC-EV administration in hospitalized patients showed enhanced oxygenation and decreased inflammatory markers, supporting their role in mitigating acute respiratory distress.30-31
“By reprogramming the immune environment, MSCs supporta regenerative state, limiting further damage from activated immune cells.”
The treatment of ischemic stroke is the most well studied ND treated with MSC-EVs. Preclinical studies demonstrated that MSC-EV treatment after ischemic stroke led to an increase in M2 macrophage, a reduction in pro-inflammatory cytokines, reduced apoptotic signalling, and an increase in angiogenesis.37 A small phase 1 trial demonstrated that MSC-EVs are safe and potentially effective in patients undergoing decompressive craniectomy.39
The versatility of MSC-EV administration is exemplified by two studies using topical delivery. Dry eye symptoms in patients with the autoimmune condition Sjogren’s syndrome showed improvements after topical application of Wharton’s jelly-derived MSC-EVs, which were accompanied by decreased levels of SASP cytokines, including IL-6, in tear fluid.36 In dermatology, ATMSC-EVs moderately reduced melanin production in hyperpigmentation disorders.38 Lastly, there are ongoing trials assessing MSC-EVs for burn wounds.40
MSC-EVs represent a paradigm shift in regenerative medicine. They capture the therapeutic benefits of MSCs while avoiding their primary safety, delivery, and manufacturing limitations. By modulating inflammation, reversing cellular senescence, and activating tissue repair pathways, MSC-EVs have demonstrated broad potential across musculoskeletal, respiratory, neurological, autoimmune, and dermatologic diseases. The MSC-EV field is now moving toward larger and more rigorous clinical trials, which will be critical for validating their safety, efficacy, and longterm benefits.

Dr. Adam Brockman, DC, ND, co-host of America’s #1 health talk radio show, nationally recognized speaker, and regenerative medicine expert is a dual-doctorate in chiropractic and naturopathy. His clinical experience ranges from founding the Complete Wellness Companies, a nationally recognized regenerative medicine practice network, to developing topical pain relief products. To contact Dr. Brockman visit NuvoCellbioloqics.com.

Dr. Sean Vandersluis earned his PhD in Biochemistry from McMaster University in 2024, where he investigated how stem cell biology underlies cancer progression. His research led to the discovery of novel therapeutics targeting cancer stem cells and the development of a personalized medicine platform based on cancer stem cell biology. To contact Dr. Vanderlsluis email [email protected]
References:
1. Niccoli T, Partridge L. Ageing as a risk factor for disease. Curr Biol. 2012 Sep ll;22(17):R741-52. doi: 10.1016/j.cub.2012.07.024. PMID: 22975005.
2. Brito KNL, Trentin AG. Role of mesenchymal stromal cell secretome on recovery from cellular senescence: an overview. Cytotherapy. 2025 Apr;27(4):422-437. doi: 10.1016/j.jcyt.2024.11.014. Epub 2024 Nov 22. PMID: 39674933.
3. Wang B, Han J, Elisseeff JH, Demaria M. The senescence-associated secretory phenotype and its physiological and pathological implications. Nat Rev Mol Cell Biol. 2024 Dec;25(12):958-978. doi: 10.1038/ s41580-024-00727-x. Epub 2024 Apr 23. PMID: 38654098.
4. Olivieri F, Prattichizzo F, Grillari J, Balistreri CR. Cellular senescence and inflammaging in age-related diseases. Mediators Inflamm. 2018 Apr 17:2018:9076485. doi: 10.1155/2018/9076485. PMID: 29849499; PMCID: PMC5932453.
5. Kou M, Huang L, Yang J, Chiang Z, Chen S, Liu J, Guo L, Zhang X, Zhou X, Xu X, Van X, Wang Y, Zhang J, Xu A, Tse HF, Lian Q. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? Cell Death Dis. 2022 Jul 4;13(7):580. doi: 10.1038/s41419-022-05034-x. PMID: 35787632; PMCID: PMC9252569.
6. Maqsood M, Kang M, Wu X, Chen J, Teng L, Qiu L. Adult mesenchymal stem cells and their exosomes: Sources, characteristics, and application in regenerative medicine. Life Sci. 2020 Sep 1:256:118002. doi: 10.1016/j.lfs.2020.118002. Epub 2020 Jun 29. PMID: 32585248.
7. Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008 Sep;8(9):726-36. doi: 10.1038/ nri2395. PMID: 19172693.
8. Jovic D, Yu Y, Wang D, Wang K, Li H, Xu F, Liu C, Liu J, Luo Y. A brief overview of global trends in MSC-based cell therapy. Stem Cell Rev Rep. 2022 Jun;18(5): 1525-1545. doi: 10.1007/sl2015-022-10369-l. Epub 2022 Mar 28. PMID: 35344199; PMCID: PMC8958818.
9. Zhou T, Yuan Z, Weng J, Pei D, Du X, He C, Lai P. Challenges and advances in clinical applications of mesenchymal stromal cells. J Hematol Oncol. 2021 Feb 12;14(1):24. doi: 10.1186/sl3045-021-01037-x. PMID: 33579329; PMCID: PMC7880217.
10. Li L, Dong L, Zhang J, Gao F, Hui J, Yan J. Mesenchymal stem cells with downregulated hippo signaling attenuate lung injury in mice with lipopolysaccharide-induced acute respiratory distress syndrome. Int J Mol Med. 2019 Mar;43(3): 1241-1252. doi: 10.3892/ijmm.2018.4047. Epub 2018 Dec 31. PMID: 30628652; PMCID: PMC6365074.
11. Maldonado M, Nam J. The role of changes in extracellular matrix of cartilage in the presence of inflammation on the pathology of osteoarthritis. Biomed Res Int. 2013:2013:284873. doi: 10.1155/2013/284873. Epub 2013 Aug 28. PMID: 24069595; PMCID: PMC3771246.
12. Lu K, Li HY, Yang K, Wu JL, Cai XW, Zhou Y, Li CQ. Exosomes as potential alternatives to stem cell therapy for intervertebral disc degeneration: in vitro study on exosomes in interaction of nucleus pulposus cells and bone marrow mesenchymal stem cells. Stem Cell Res Ther. 2017 May 10;8(l):108. doi: 10.1186/sl3287-017-0563-9. PMID: 28486958; PMCID: PMC5424403.
13. Gao Y, Liu MF, Li Y, Liu X, Cao YJ, Long QF, Yu J, Li JY. Mesenchymal stem cells-extracellular vesicles alleviate pulmonary fibrosis by regulating immunomodulators. World J Stem Cells. 2024 Jun 26;16(6):670-689. doi: 10.4252/wjsc.vl6.i6.670. PMID: 38948098; PMCID: PMC11212550.
14. Zhang S, Chuah SJ, Lai RC, Hui JHP, Lim SK, Toh WS. MSC exosomes mediate cartilage repair by enhancing proliferation, attenuating apoptosis and modulating immune reactivity. Biomaterials. 2018 Feb;156:16-27. doi: 10.1016/j.biomaterials.2017.11.028. Epub 2017 Nov 21. PMID: 29182933.
15. Li S, Stockl S, Lukas C, Gotz J, Herrmann M, Federlin M, Grassel S. hBMSC-Derived extracellular vesicles attenuate IL-ip-Induced catabolic effects on OA-chondrocytes by regulating pro-inflammatory signaling pathways. Front Bioeng Biotechnol. 2020 Dec 14:8:603598. doi: 10.3389/fbioe.2020.603598. PMID: 33425869; PMCID: PMC7793861.
16. Zhou Y, Wen LL, Li YF, Wu KM, Duan RR, Yao YB, Jing LJ, Gong Z, Teng JF, Jia YJ. Exosomes derived from bone marrow mesenchymal stem cells protect the injured spinal cord by inhibiting pericyte pyroptosis. Neural Regen Res. 2022 Jan;17(l): 194-202. doi: 10.4103/16735374.314323. PMID: 34100456; PMCID: PMC8451579.
17. Wang L, Wu Y, Yao R, Li Y, Wei Y, CaoY, ZhangZ,WuM, ZhuH, Yao Y, Kang H. The role of mesenchymal stem cell-derived extracellular vesicles in inflammation-associated programmed cell death. Nano Today. 2023 June;50:101865. https://doi.Org/10.1016/j.nantod.2023.101865.
18. Lightner AL, Sengupta V, Qian S, Ransom JT, Suzuki S, Park DJ, Melson TI, Williams BP, Walsh JJ, Awili M. Bone marrow mesenchymal stem cell-derived extracellular vesicle infusion for the treatment of respiratory failure from COVID-19: a randomized, placebo-controlled dosing clinical trial. Chest. 2023 Dec;164(6): 1444-1453. doi: 10.1016/j.chest.2023.06.024. Epub 2023 Jun 23. Erratum in: Chest. 2024 Jul;166(l):240. doi: 10.1016/j.chest.2024.05.003. PMID: 37356708; PMCID: PMC10289818.
19. Kaffash Farkhad N, Sedaghat A, Reihani H, Adhami Moghadam A, Bagheri Moghadam A, Khadem Ghaebi N, Khodadoust MA, Ganjali R, Tafreshian AR, Tavakol-Afshari J. Mesenchymal stromal cell therapy for COVID-19-induced ARDS patients: a successful phase 1, control-placebo group, clinical trial. Stem Cell Res Ther. 2022 Jun 28;13(1):283. doi: 10.1186/sl 3287-022-02920-1. PMID: 35765103; PMCID: PMC9241239.
20. Ghasemi M, Roshandel E, Mohammadian M, Farhadihosseinabadi B, Akbarzadehlaleh P, Shamsasenjan K. Mesenchymal stromal cell-derived secretome-based therapy for neurodegenerative diseases: overview of clinical trials. Stem Cell Res Ther. 2023 May 4;14(1):122. doi: 10.1186/ si3287-023-03264-0. PMID: 37143147; PMCID: PMC10161443.
21. Manferdini C, Paolella F, Gabusi E, Silvestri Y, Gambari L, Cattini L, Filardo G, Fleury-Cappellesso S, Lisignoli G. From osteoarthritic synovium to synovial-derived cells characterization: synovial macrophages are key effector cells. Arthritis Res Ther. 2016 Apr 4;18:83. doi: 10.1186/ S13075-016-0983-4. PMID: 27044395; PMCID: PMC4820904.
22. Cosenza S, Toupet K, Maumus M, Luz-Crawford P, Blanc-Brude O, Jorgensen C, Noel D. Mesenchymal stem cells-derived exosomes are more immunosuppressive than microparticles in inflammatory arthritis. Theranostics. 2018 Feb 3;8(5): 1399-1410. doi: 10.7150/thno.21072. PMID: 29507629; PMCID: PMC5835945.
23. Wang Y, Kong Y, Du J, Qi L, Liu M, Xie S, Hao J, Li M, Cao S, Cui H, Liu A, Ma J, Song Y. Injection of human umbilical cord mesenchymal stem cells exosomes for the treatment of knee osteoarthritis: from preclinical to clinical research. JTransl Med. 2025 Jun 11;23(1):641. doi: 10.1186/ sl2967-025-06623-y. PMID: 40500748; PMCID: PMC12153132.
24. Habibi A, Khosravi A, Soleimani M, Nejabat M, Dara M, Azarpira N. Efficacy of topical mesenchymal stem cell exosome in Sjogren's syndrome-related dry eye: a randomized clinical trial. BMC Ophthalmol. 2025 May 20;25(l):299. doi: 10.1186/sl2886-025-04078-9. PMID: 40394561; PMCID: PMC 12090426.
25. Chen KH, Chen CH, Wallace CG, Yuen CM, Kao GS, Chen YL, Shao PL, Chen YL, Chai HT, Lin KC, Liu CF, Chang HW, Lee MS, Yip HK. Intravenous administration of xenogenic adipose-derived mesenchymal stem cells (ADMSC) and ADMSC-derived exosomes markedly reduced brain infarct volume and preserved neurological function in rat after acute ischemic stroke. Oncotarget. 2016 Nov 15;7(46):74537-74556. doi: 10.18632/oncotarget. 12902. PMID: 27793019; PMCID: PMC5342685.
*See more references (26-40) online.
 View Full Issue
View Full Issue