5 Core Practice Management Metrics That Create Better Care and Stronger Practices
February 1 2026 Christopher J. Colloca5 Core Practice Management Metrics That Create Better Care and Stronger Practices
February 1 2026 Christopher J. Colloca
IF YOU CAN MEASURE IT, YOU CAN MANAGE IT.
WITHOUT QUANTIFIABLE DATA ON THE PERFORMANCE OF OUR PRACtices, we are simply guessing about the quality of our care and the success of our practices.
Most doctors of chiropractic (DCs) didn’t enter the profession because they love spreadsheets, however. They entered it to help people move better, feel better, and live better. I get it. Yet, the reality of modern practice is this: the quality of care delivered in a chiropractic office is inseparable from how well that office is managed and the kind of information that is collected and interpreted.
Across healthcare, be it medicine, dentistry, or physical therapy, successful practices have learned a simple lesson: what gets measured can be improved, and what gets improved protects both patients and providers. For chiropractors, practice-management statistics are not about becoming “corporate.” They are about creating clarity in a system where time, attention, and energy are finite.
When numbers are ignored, stress fills the gap, we guess, and chaos ensues. When numbers are understood, practices become calmer, more predictable, and more patient-centered.
A chiropractic clinic is a time-based professional service business. Rent, salaries, equipment, and software are largely fixed costs. Once those costs are paid, the difference between a stable profitable practice and a chaotic, exhausting one often comes down to how well appointment time is used.
In healthcare economics, unused appointment slots are described as perishable inventory. A missed visit cannot be stored and sold later. It disappears, taking potential revenue, staff productivity, and continuity of care along with it.
That is why medical groups, dental practices, and physical therapy clinics closely track access, visit volume, cancellations, and throughput. Chiropractors who adopt the same discipline gain control over their schedules, reduce burnout, and improve patient outcomes. Let’s do a shallow dive into each of the five most important core metrics that every practice must track at the very minimum.
What the number tells you
New patient counts are a leading indicator of future growth. They reflect how visible, accessible, and trusted the practice is in its community.
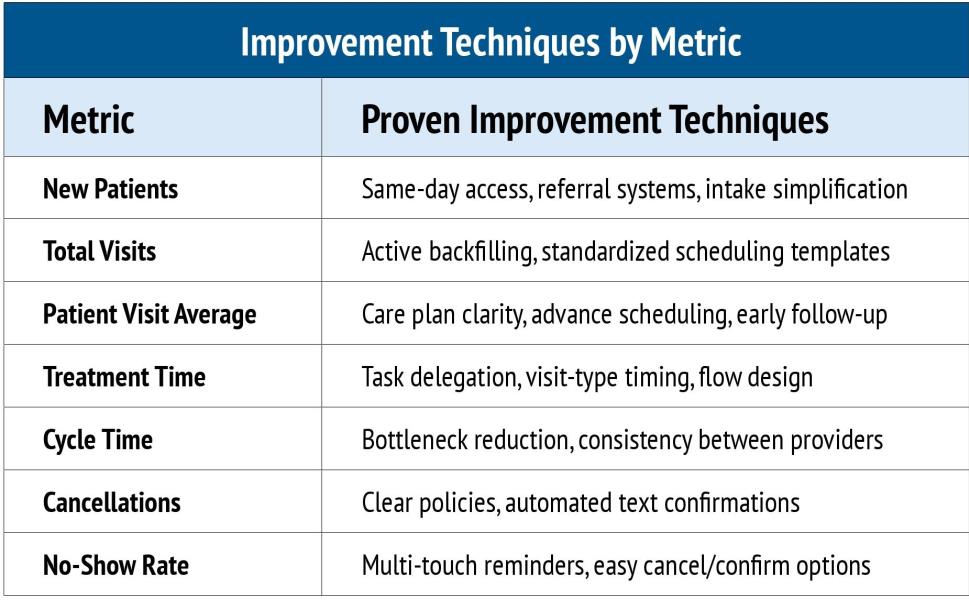
How high-performing practices improve it
Successful healthcare practices don’t rely on luck or a single referral source. They build systems for demand.
• Reduce friction at the front door:
Patients are more likely to schedule—and keep—appointments when intake is simple. Online forms, clear instructions, and friendly, confident scheduling conversations matter.
“Regardless of the profession, practice metrics are no longer viewed as “business tools.” They are viewed as caredelivery tools.”
Weekly 30-Minute Staff Meeting Agenda
• New patients (actual vs goal)
• Total visits
• Cancellation & no-show rate
• Open slots next 7 days
• One system improvement for the coming week
• Consistency matters more than perfection.
Core Chiropractic Practice Metrics (Quick Reference)
• Protect access: Same-day or nextday availability for new patients dramatically improves conversion from inquiry to visit.
• Diversify referral sources: Internal referrals, professional referrals, online visibility, and community relationships each stabilize demand.
• Track conversion, not just inquiries: If phone calls or website leads increase but new patient visits do not, the issue is often scheduling confidence or access—not marketing.
Patients don’t decide to seek care when it’s convenient for the clinic. They decide when pain or concern reaches a tipping point. Practices that meet patients at that moment earn trust before the first adjustment.
What the number tells you
Total visits reflect how well the practice converts demand into actual care. It also reveals whether the clinic’s capacity is aligned with patient flow.
• Treat the schedule like inventory: Every open slot has value. Practices that assign responsibility for filling cancellations protect revenue and continuity.
• Create a short-notice fill system: Maintain a list of patients who welcome earlier appointments and contact them when openings appear.
• Standardize appointment types: Improve flow by having assistants help where possible under your state law to improve efficiency in financial reports of findings, physical examinations, radiographs, exams and re-exams, and therapy. Be sure to define realistic time blocks for your flow.
A full schedule does not always mean a productive day. Predictable flow— rather than frantic busyness—is what keeps teams energized and patients feeling cared for.
PVA equals the number of patient visits divided by the number of new patients for a given period (month, quarter, year, career). Visit average reflects how well patients understand, value, and follow recommended care. It is one of the clearest indicators of patient engagement and the retention of a practice.
“Booking multiple visits in advance during active care plans emphasizes priority, reduces drop-off and decision fatigue.”
• Clarify expectations early: Patients are more likely to stay when care plans include clear goals, timelines, and reassessment points.
• Schedule ahead: Booking multiple visits in advance during active care plans emphasizes priority, reduces drop-off and decision fatigue.
• Address missed visits immediately:
Early follow-up prevents small interruptions from becoming permanent disengagement.
• Pair visit averages with outcomes:
Tracking progress ensures that visit averages reflect value, not inertia.
Most patients don’t “quit” care, they drift away when the importance of care is not communicated, expectations are unclear, and results are lacking. Practices that guide patients with clarity remove uncertainty and build confidence.
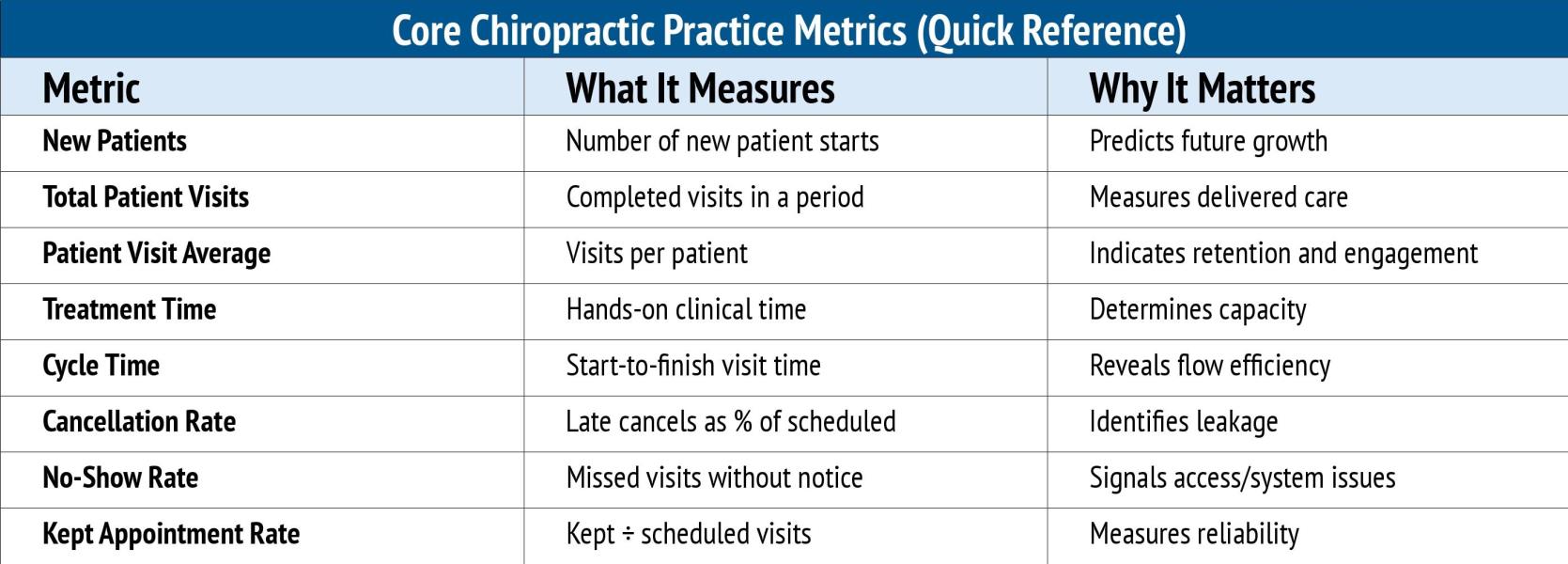
Treatment time and cycle time show how efficiently care is delivered and whether the practice can grow without adding stress or hours.
• Measure reality, not assumptions: Identify where bottlenecks occur in your patient flow.
• Reduce variation: Consistency matters more than speed. Predictable visit flow keeps schedules on time and manages expectations.
• Separate clinical from non-clinical tasks: Delegating appropriate duties to staff members improves provider focus and patient experience.
• Design for flow: Patient movement through the clinic should feel smooth, not hurried.
Patients don’t mind efficient care, but they do notice chaos. A calm, predictable visit experience builds confidence and trust.
Track cancellations and no-shows separately and as a percentage as compared to total scheduled and kept appointments. Missed appointments reveal how well expectations are set, reminders are managed, and relationships are maintained.
• Set expectations clearly and kindly: Policies work best when they are communicated early and consistently
• Use automated text reminders with confirmation requests: Combining verbal reminders at checkout with automated texts or emails increases reliability. Text messages that allow patients to confirm or cancel reduce no-shows by prompting action rather than passive reminders.
• Track kept appointment rate: Focusing on successful visits reinforces positive systems rather than frustration.
Most missed appointments are not acts of disrespect. They are acts of distraction. Good systems protect patients from their own busy lives and communicate the importance of patient compliance with results.
The “Kept Appointment Rate” Formula
Kept Appointment Rate = Completed Visits T Scheduled Visits x 100
Why it matters:
• Shifts focus from blame to system performance
• Aligns staff behavior with success
• Reflects real operational health
• High-performing practices aim to improve this number steadily, not perfectly.
Sample Automated Text Reminder (Best Practice)
“Hi [Patient Name], this is a reminder of your appointment at [Practice Name] on [Date] at [Time], Reply YES to confirm or C to cancel. We look forward to seeing you!”
Why it works:
• Requires active confirmation
• Gives patients control
• Reduces forgotten appointments
Beyond the core numbers, high-functioning practices also monitor:
• Access and availability (days to next appointment)
• Capacity utilization (provider and room usage)
• Revenue per visit and per hour
• Patient satisfaction and outcomes
Together, these metrics form a feedback loop that guides staffing, scheduling, and growth decisions.
Regardless of the profession, practice metrics are no longer viewed as “business tools.” They are viewed as care-delivery tools. They ensure patients are seen on time, plans are followed, teams are supported, and clinicians can focus on what they do best. Reviewing daily, weekly, monthly, and yearly practice statistics enables you set goals and monitor the health of your business.
Tracking and improving the right numbers creates something invaluable: better planning, improved expectations management, less stress, smoother patient continuity, more predictable income, and a consistent practice that feels intentional rather than reactive. Begin with these five core metrics and watch your practice grow.

Dr. Christopher Colloca is a chiropractic scientist and innovator regarded as the world’s leading authority on instrument adjusting. He is the CEO and Founder of Neuromechanical Innovations, a FDA registered medical device manufacturer of the Impulse® family of instruments that are in use in over 20,000 clinics in over 50 countries delivering over 750 million adjustments annually worldwide. His award-winning research has been published in over 50 scientific journal articles and among his intellectual property are more than 30 patents and trademarks. Chris travels the globe training thousands of doctors in his techniques and technologies each year. He can be reached at [email protected] or visit www.Neuromechanical.com.
1. Berwick, D. M., Nolan, T. W, & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759-769.
2. Bodenheimer, T, & Pham, H. H. (2010). Primary care: Current problems and proposed solutions. Health Affairs, 29(5), 799-805.
3. Green, L. V, Savin, S„ & Lu, Y. (2013). Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Affairs, 32(1), 11-19.
4. Institute for Healthcare Improvement. (2020). Improving access to primary care. IHI White Paper.
5. Kaplan, R. S„ & Porter, ME. (2011). How to solve the cost crisis in health care. Harvard Business Review, 89(9), 46-52.
6. MGMA. (2023). Performance and practices of successful medical groups. Medical Group Management Association.
7. Neely, A., Gregory, M., & Platts, K. (2005). Performance measurement system design: A literature review and research agenda. International Journal of Operations & Production Management, 25(12), 1228-1263.
8. Porter, M. E. (2010). What is value in health care? New England Journal of Medicine, 363(26), 2477-2481.
9. Smith, M., Saunders, R., Stuckhardt, L., & McGinnis, J. M. (Eds.). (2013). Best care at lower cost: The path to continuously learning health care in America. National Academies Press.
10. Wiler, J. L., Bolandifar, E., Griffey, R. T, Poirier, R. F., & Olsen, T. (2013). An emergency department patient flow model based on queueing theory principles. Academic Emergency Medicine, 20(9), 939-946.
 View Full Issue
View Full Issue