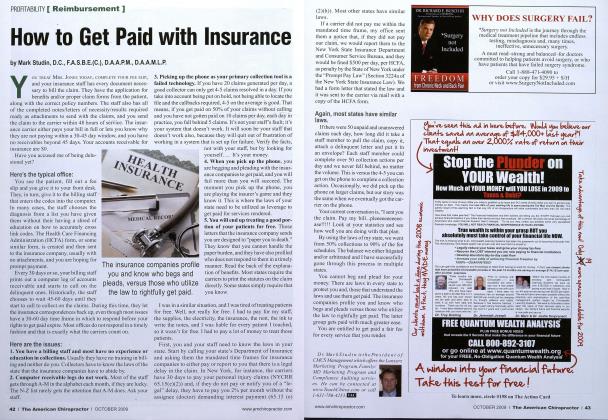
■ TWO SUBSIDIARIES OF UNITED HEALTH- care, based in St. Louis, will pay $536,000 in fines and reopen chiropractic claim files it has denied since 2004. Under a settlement with the Missouri Department of Insurance, United Healthcare has agreed to reexamine at least 50,000 claims filed by chiropractors who treated the company's policyholders. The Department of Insurance found United Healthcare violated state insurance laws by limiting coverage to 26 visits per year. In other cases, the department says the company failed to evaluate the medical necessity of treatment before denying claims. For any chiropractic claims it finds were improperly denied, United Healthcare must reimburse the physicians for those claims, plus interest. In some cases, consumers may have paid the bills, rather than the chiropractors. Those consumers should contact United Healthcare at 1-800-873-4575. Patients or chiropractors with questions about the settlement can call the Department of Insurance Consumer Hotline at 1-800-726-7390 or visit insurance.mo.gov. The department conducts 30 to 40 market conduct exams of insurance companies in a typical year and, in 2008, these exams yielded more than $6 million in restitution for consumers and -more than S700,000 in fines to benefit Missouri public schools. The Department of Insurance can order a market conduct exam at any time, if it suspects violations of Missouri insurance laws. For further information, contact The Public Information Office at 1-573-751-2562.
 View Full Issue
View Full Issue