Initial Visit Productivity
PRACTICE MANAGEMENT
K. Jeffrey Miller
New patients are the lifeblood of most chiropractic practices. In turn, a patient’s first two visits are of the utmost importance because the evaluation and report of findings occur during these visits. Most doctors render thorough examinations for the techniques they use, and most provide effective reports of findings. However, many do not involve clinical staff in a manner that would make the initial visit more productive.
Most clinical staff members aie utilized for treatment procedures, such as applying passive therapies or assisting with active rehabilitation procedures. Some clinical staff members have limited radiation certifications that allow them to take and process radiographs. A radiation certification expands the average clinical staff member’s role beyond therapeutic procedures into participation in the diagnostic process. Many doctors are not applying this expansion in the most productive manner. Expansion is possible here for all clinical staff, whether they aie only involved in therapeutic processes or have a limited radiation certification. The easiest route for increasing initial visit productivity is to involve clinical staff in the examination. Clinical staff can perform several examination procedures. The easiest route for increasing initial visit productivity is to involve clinical staff in the examination. While this statement is good news, a short disclaimer must accompany it. Chiropractic scope of practice varies from state to state. Each doctor must be well versed in the regulations regarding the job descriptions for chiropractic staff members.
Two situations aie common among the different states. First, staff may participate in examination procedures only if trained to do so through a state-approved chiropractic assistant certification program. Second, the staff may participate in examination procedures that involve obtaining physical measurements. To be safe, we will focus on the situation where any clinical staff member can take measurements and record them. Procedures that involve measurements do not require immediate interpretation. Staff can obtain the physical measurements and record them for the doctor to interpret along with other findings. The first eight procedures in Table 1 under Routine Physical Measurements aie the common vital signs used in all healthcare fields. The ninth, “pain scales,” has not traditionally been considered a vital sign and its inclusion is recent.
The next four vital signs ai e the most pertinent to chiropractic evaluations and techniques. Grip strength is used intermittently, and may or may not be appropriate to the patient’s situation.
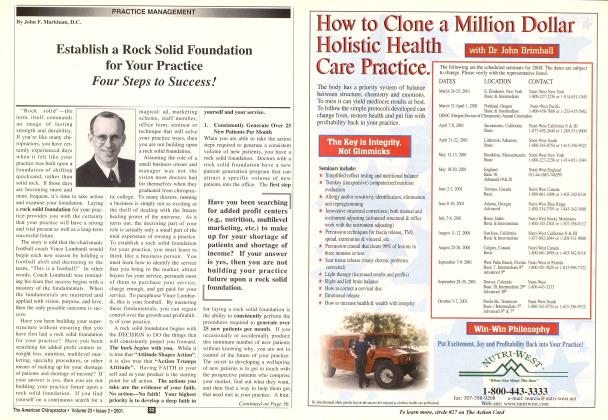
Table 1 lists examination procedures that are routine physical measurements. Routine Physical Measurements Height Weight Temperature Blood pressure Sitting Recumbent Standing Pulse rate Respiration rate Pain scales Biomechanical scanning for orthotic need Postural analysis Range of motion Grip strength
Table 1 Examination Procedure Based on Physical Measurements Pertinent Chiropractic Physical Measurements Pain scales Biomechanical scanning for orthotic need Postmal analysis Range of motion Height Weight Blood pressure Temperature
Height, weight, blood pressure, and temperature are the four common vital signs most pertinent to chiropractic treatment.
Pain Scales: Pain scales are great for tracking the severity of a patient’s pain as well as progress or lack of progress. Medicare and most third-party payers also require them for clinical documentation.
Biomechanical Scanning for Orthotic Need: The foundation for postural and biomechanical analysis begins at the body’s musculoskeletal foundation—the feet. If the feet pronate excessively, have valgus positioning (toeing out), have fallen arches, and/or have Achilles tendons that bow medially, there will be corresponding biomechanical faults above the feet. The feet affect all knee, hip, pelvic, spinal, and head postures.
Scanning the feet helps confirm findings and effects associated with the physical findings at the feet. Scanning also provides images that ai e of great benefit during the report of findings. Foot scanning often confuses patients. They sometimes have trouble making the connection between their feet and any complaints they have higher up in the biomechanical chain. This is where the images and educational materials provided by scanning systems aie invaluable. Doctors failing to start
postural and biomechanical examinations at the feet aie starting in the middle of these examinations. This can result in limiting the effectiveness of some aspects of the patient’s care. Since understanding foot scanning is a stretch for some patients, and it often leads to the selling of a product in addition to adjustments, staff must be trained to answer basic questions regarding the reasoning behind the scans and the products associated with them.
Postural Analysis: Beyond analysis of the feet, the body should be assessed from the anterior, posterior, and lateral aspects. The knees should be assessed for valgus and varus positioning. Hyperextension or failure to completely extend should also be investigated. The hips should be assessed for excessive internal or external rotation as well as trochanteric height. The pelvis should be assessed for obliquity and anterior or posterior tilting. Spinal curves should be inspected for excessive lordosis or kyphosis. Examination for scoliosis is also employed. Additional observations for shoulder height, head tilt, and anterior head translation should also occur. These findings have traditionally been observed. However, multiple computer systems and apps are now available for use. Just like the images and educational materials provided by foot scanning systems, images from postural analysis systems make the report of findings much more understandable and effective.
Range of Motion: Multiple methods exist for range of motion measurement. Ranges can be observed for spinal and extremity joints. Spinal ranges can be measured by mechanical or electronic inclinometers. Extremity ranges can be measured by goniometers. Range of motion assessment is the most commonly used measurement pertinent to chiropractic care. In consideration of this, the only tips offered concern the numbers used as normal for each joint’s normal ranges. The ranges listed as normal for each joint often differ from text to text. To address this situation, it is recommended that the numbers used in the American Medical
Association’s Guides to the Evaluation of Permanent Impairment be used because information from the guides is often the final word in healthcare cases that involve litigation. Additionally, doctors must remember that ranges of motion vary with age and gender.
Height and Weight: The relationship of height and weight in determination of BMI, strain on the musculoskeletal system, and just general health are well documented. Minimal explanation is necessary here.
Blood Pressure: High blood pressure is a common health factor related to heart disease, kidney disease, stroke, stress, and many other serious conditions. Even if the doctor of chiropractic does not choose to be involved in the regulation of a patient’s blood pressure, he or she should be involved in the screening and monitoring of all patients’ blood pressure.
Temperature: Infections and other pathologies of the upper respiratory system, lungs, pelvis, kidneys, and other organs or regions can result in neck and/or back pain. This makes assessing temperature an important initial procedure. There are several new technologies being utilized for temperature measure that make the process quick and painless.
At this point, it should be obvious that training clinical staff members in the proper use of procedures involving physical measurements is a good idea. It provides several important improvements within a practice. Parts of the examination are removed from the doctor’s responsibility, providing the doctor with additional free time. More procedures may be performed as part of the initial examination with staff involvement. This could lead to increased diagnostic information. Finally, additional avenues can be explored for implementation in the doctor’s plan of care for a patient.
K. Jeffrey Miller, DC, MBA is a " ça chiropractic orthopedist in Roanoke, VA, Dr. Miller is the author of Prcicticcil Assessment of the Chiropractic Patient, Orthopedic and Neurological Examination in a Flash, Chiropractic Medicare Documentation Self Inventory and The Road to Happiness is Always Under Construction. He can be reached through his website examdoc.com
 View Full Issue
View Full Issue