The Mechanism of the Chiropractic Spinal Adjustment/Manipulation: Subluxation Degeneration
FEATURE
Effect of Sagittal Alignment on Kinematic Changes and Degree of Disc Degeneration in the Lumbar Spine
Part Four of a Five-Part Series
Mark Studin
DC, FASBE(C), DAAPM, DAAMLP
William J. Owens
DC, DAAMLP
More evidence is coming forward that demonstrates both spinal stability and biomechanical balance as an important aspect of spine care. The good news is that this is well within chiropractic’s scope, but many doctors of chiropractic are missing the education to accurately evaluate and objectify these types of biomechanical lesions. Our profession has spent most of the past 122 years focused on treating these biomechanical lesions (vertebral subluxation, joint fixation, etc.) with little regaid to the ’‘assessment” component. The reason that is a critical statement is that we treat compensation versus the unstable joint too often.
Our founding doctors had used very specific techniques to analyze the spine h orn a functional perspective, and most of our contemporary treatment techniques came out of these analyses, which are the basis for many of the most common techniques taught in today’s chiropractic academia. In hindsight, it seems that die major discussions of the time (early chiropractic) were about “identification” of the lesion to adjust, and then evolved into the best way to deliver the adjustment.
Our roots and subsequently the true value and expertise of the doctor of chiropractic is in the assessment with treatment secondary to an accurate diagnosis. The medical community that we [and the doctors we train] teach no longer confuse our delivering of chiropractic care with a physical therapy manipulation or mobilization. One significant reason; our focus is on the diagnosis, prognosis and treatment plan BEFORE we render our treatment moving us away horn behig a technician or secondary provider.
With medical specialists who understand the spine, our conversation centers on sphial biomechanics and how a specific chiropractic spinal adjustment will restore sagittal/coronal alignment and coupled motion balance the spine. We discuss spinal biomechanics and have the literature and credentials to validate
our diagnosis, prognosis, and treatment plan. Chiropractic has been the leader in this treatment for more than a century, but since we chose to stay outside of die mainstream healthcare system, we had no platform to take a leadership position or be heard.
Medicine at both the academic and clinical levels is embracing chiropractic as the primary solution to mechanical spine issues (no fracture, tumor, or infection) because, as one primary care provider shared with us, “traditional medical therapies inclusive of physical therapy have no basis in reality in how to treat these patients, which has led us, in part, to the opiate crisis.” Part of the validation of what chiropractic offers in a biomechanical paradigm comes horn surgical journals in the medical community.
Keorochana et al. (2011) published a paper in Spine titled “To determine the effects of total sagittal lordosis on spinal kinematics and degree of disc degeneration in the lumbar spine: An analysis using positional MRI.” Remember that this article
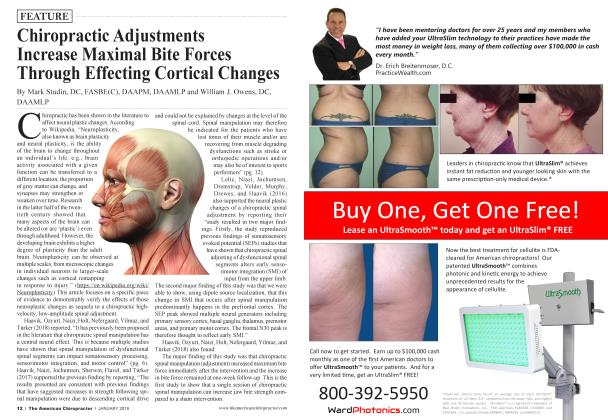
Appendix A Grade Structure Distinction Signal Height of of nucleus Intensity intervertebral and annulus disc I Homogenous, •moge: Clear Hyperintense, Normal :iglit w isointense to cerebrospinal fluid II Inhomogenous Clear Hyperintense, Normal with or widiout cerebrospinal isointense to horizontal bands mrospu fluid III Inhomogenous, Unclear Intermediate Normal grey to slightly decreased IY Inhomogenous, Intermediate Normal to grey to Flack to hypointense moderately decreased V Inhomogenous, Hypointense Collapsed disc space
*Adapted from Pfirmann et al. (2001) (8)
Note. Teichtahl, A. J., Urquhart, D. M., Wang, Y., Wluka, A. E., Heritier, S. & Cicuttini, F. M. (2015). A dose-response relationship between severity of disc degeneration and intervertebral disc height in the lumbosacral spine. Arthritis Research & Therapy, 17(297). Retrieved from https://openi.nhn.nih.gov/ detailedresult.php?img= PMC4619538_13075_2015_820_Figl_ HTML&req=4
was written eight years ago and, as a concept, has evolved considerably since it was first discussed in the late 1990s. This is the clinical component of what Panjabi had successfully described and reproduced in the laboratory. It is now starting to become mainstream in clinical practice.
Many people ask why surgeons would care about the biomechanics of the spine when they are looking simply for an anatomical lesion to stabilize (fracture, tumor, infection, cord compression). The authors answer this question by statmg, “It has also been a topic of great interest in the management of lumbar degenerative pathologies, especially when focusing on the role it may play in accelerating adjacent degeneration after spinal fusion and non-fusion procedures, such as dynamic stabilization and total disc replacement” (p. 893).
They continue by stating, “Alterations in the stress distribution may ultimately influence the occurrence of spinal degeneration. Moreover, changes in sagittal morphology may alter the mechanics of the lumbar spine, affecting mobility. Nevertheless, the relationships of sagittal alignment on lumbar degeneration and segmental motion have not been fully defined” (p. 893). This is precisely what our founding fathers called “subluxation and subluxation degeneration!”
Regarding the type and number of patients in the study, the authors reported that “pMRIs [positional MRI] of the lumbar spine were obtained for 430 consecutive patients (241 males and 189 females) from February 2007 to February 2008. All patients were referred for pMRI [positional MRI, which included compression in both flexion and extension with a particular focus on segmentation translation and angular motions] due to complaints of low back pain with or without leg pain” (p. 894). This is the part where they looked for hypermobility.
In the first step in the analysis, the authors reviewed data regarding the global sagittal curvature, as well as the individual angular segmental contributions to the curvature. The next step
involved the classification of the seventy of lumbar disc degeneration using the Pfirrmann classification system (see Appendix A if you are not familiar). This is where they looked for segmental degeneration. The patients were then classified based on the lordosis angle (T12-S1). The groups were as follows:
Group A - Straight spine or kyphosis - (lordosis angle 20°) Group B - Nonnal lordosis - (lordosis angle 20° to 50°) Group C - Hyperlordosis - (lordosis angle 50°)
Appendix B
Note. Teraguclii, M., Yoshimura, N., Hashizume, H., Muraki, S., Yamada, H., Minamide, A., Oka, H., Ishimoto, Y, Nagata, K. Kagotani, R., Takiguchi, N., Akune, T., Kawaguchi, H., Nakamura, K., & Yoshida, M. (2014). Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthritis and Cartilage, 22(1). Retrieved from http://www.sciencedirect.com/science/ article/pii/ S1063458413010029
Figure 7 - Disc classification, visual classification model for intervertebral disc as I to Y.
Note. Puertas, E. B., Yamashita, H., Manoel de Oliveira, V., & Satiro de Souza, P. (2009). Classification of intervertebral disc degeneration by magnetic resonance. Acta Ortopedica Brasileira, 17(1). Retrieved from http://www.scielo.br/scielo.plip?pid=S141378522009000100009&script=sci_arttextlng=en
There is a structural categorization (lordosis) and a degenerative categorization (Pfirrmann) in this paper, and the authors sought to see if there was a predictable relationship.
The results of this study were interesting and validated much of what the chiropractic profession has discussed relating to segmental '‘compensation” in the spine. Meaning, when one segment is hypomobile, adjacent segments will increase motility to compensate. The authors stated, “The sagittal lumbar spine curvature has been established as an important parameter when evaluating intervertebral disc loads and stresses in both clinical and cadaveric biomechanical investigations” (p. 896). They continue by stating, “In vitro [in the laboratory or outside of the living organism] biomechanical tests do not take into account the influence of ligaments and musculature, and may not adequately address the complex biomechanics of the spine” (p. 896).
When it comes to spinal balance and distribution of loads in the spine, the authors reported, “Our results may indicate that the
border segments of lordosis, especially in the upper lumbar spine (L1-L2, L2-L3, and L3-L4), have greater motion in straight or kyphotic spines, and less segmental motion in hyperlordotic patients” (p. 896).
They continued by stating, “A greater degree of rigidity is found at the apical portion of straight or kyphotic spines, and more mobility is seen at the apical portion of hyperlordotic spines” (p. 897). Therefore, in both cases, we see that changes in the sagittal configuration of the human spine have consequences for the individual segments involved.
This raises the question: How does this relate to accelerated degeneration of the motion segments involved? (subluxation degeneration) The authors reported, “Regarding the relationship
between the degree of disc degeneration and posture, subjects with straight or kyphotic sphies tended to have a greater degree of disc degeneration at border segments, with statistical significance in the lower spine (L5-S1). On the other hand, hyperlordotic spines had a significantly greater degree of disc degeneration at the apex and upper spine (L4-L5 and L1-L2). The severity of disc degeneration tended to increase with increased mobility at the segments predisposed to greater degeneration (border segments of straight or kyphotic spines and apical segments of hyperlordotic spines)” (p. 897).
Scientific literature and medicine are now validating (proving) what chiropractic has championed for more than 122 years— that the human spine is a living neurobiomechanical entity, which responds to the changes in the external enviromnent and compensates perpetually seeking a homeostatic equilibrium. We can now have verification that changes or compensation within the spinal system as a result of a bio-neuro-mechanical lesion (vertebral subluxation) results in degeneration (subluxation degeneration) of individual motion segments.
In conclusion, the authors state:
“Changes in sagittal alignment may lead to kinematic changes and influence load bearing and the distribution of disc degeneration at each level” (p. 897).
“Sagittal alignment may alter spinal load and mobility, possibly influencing segmental degeneration” (p. 897).
“Motion and the segmental contribution to the total mobility tended to be lower at the border of lordosis, especially at the upper segments, and higher at the apex of lordosis in more lordotic spines, whereas the opposite was seen in straight or kyphotic spines” (p. 897).
Although medicine is addressing this at the surgical level, as a profession they realize they have no conservative solutions. This has “opened the door” for the credentialed doctor of chiropractic to be in a leadership role in both teaching medicine about the role of the chiropractor as the primary spine care provider and the central focus of the care path for mechanical spine issues.
When communicating with patients and medical professionals, it is critically important to educate them on what “current research” is showing and why it is important that this chiropractic approach
to spine care is the future of spine care in the United States.
References:
1. Keorochana, G., Taghavi, C. E., Lee, K. B., Yoo, J. H., Liao, J. C., Fei, Z, & Wang, J. C. (2011). Effect of sagittal alignment on kinematic changes and degree of disc degeneration in the lumbar spine: An analysis using positional MRI. Spine, 36(11), 893-898.
2. Teichtahl, A. J., Urquhart, D. M., Wang, Y., Wluka, A. E., Heri-
tier, S. & Cicuttini, F. M. (2015). A dose-response relationship between severity of disc degeneration and intervertebral disc height in the lumbosacral spine. Arthritis Research & Therapy, 17(297). Retrieved from https: openi.nlm.nih.gov/ detailedresult.php?img=PMC4619538 13075 2015 820 Figl HTML&req=4
3. Teraguchi, M., Yoshimura, N, Hashizume, H., Muraki, S., Yamada, H., Minamide, A., Oka, H., Ishimoto, Y., Nagata, K. Kagotani, R, Takiguchi, N.,Akune, T., Kawaguchi, H., Nakamura, K, & Yoshida, M. (2014). Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthritis and Cartilage, 22(1). Retrieved from http://www. sciencedirect. com/science/article/pii/S1063458413010029
4. Puertas, E. B., Yamashita, H., Manoel de Oliveira, V, & Satiro de Souza, P. (2009). Classification of intervertebral disc degeneration by magnetic resonance. Acta Ortopedica Brasileira, 17(1). Retrieved from http://www.scielo.br/ scielo.php?pid=S1413-78522009000100009&script=sci arttext&tlng=en.
fEyi. ; Dr. Mark Studin is an adjunct associate professor of ™™iP chiropractic at the University of Bridgeport College of Chiropractic; an adjunct professor of clinical sci’ J ences at Texas Chiropractic College; and a clinical “ presenter for the State of New York at Buffalo, School of Medicine and Biomedical Sciences for postdoctoral education, teaching MRI spine interpretation, spinal biomechanical engineering, and triaging trauma cases. He also coordinates a clinical rotation in neuroradiology for chiropractic students at the State University of New York at Stony Brook, School of Medicine, Department of Radiology. Dr. Studin is also the president of the Academy of Chiropractic, teaching doctors of chiropractic how to interface with the medical and legal communities (www.DoctorsPIProgram.com). He teaches MRI interpretation and triaging trauma cases to doctors of all disciplines nationally and studies trends in health care on a national scale (www.TeachDoctors.com). He can be reached at DrMark a AcademyofC'hiropractic.com or at 631-786-4253.
Dr. Bill Owens is presently in private practice in Buffalo and Rochester, New York and generates the majority of his new-patient referrals directly ■i PN JM from the primary care medical community. He is an associate adjunct professor at the State University of New York at Buffalo School of Medicine and Biomedical Sciences as well as the University of Bridgeport, College of Chiropractic, and an adjunct professor of clinical sciences at Texas Chiropractic College. He also works directly with doctors of chiropractic to help them build relationships with medical providers in their community. He can be reached at dr. owensfiacademyofchiropractic, com, via www.mdreferralprogram.com, or at 716-228-3847.
 View Full Issue
View Full Issue