To Point or Not to Point: That is the Question!
INSURANCE CODING
Kathy Mills Chang
Rhonda Hodge
MCS-P, CCPC, CCCA, and
MCS-P
With the advancement of technology, we are fortunate to have a myriad of software systems to assist in many aspects of a medical office. There are programs to help make the process of verifying benefits easier and less time-consuming than it was even ten years ago. There is technology giving providers the ability to document at a higher level than ever before. What would have been four or five pages of handwritten notes years ago can now be documented in a matter of minutes with a few simple clicks! One of the best technological advancements is the speed and accuracy at which claims can be billed to and paid by insurance carriers. Before the days of electronic billing, claims were sent through the postal service, and it took three to four weeks or longer to receive a response. Today, that turnaround time is one to two weeks and payment is deposited automatically. Gone are the days of handwritten claim forms or waiting for the printer to spit them out, reviewing and making corrections, addressing envelopes, and then heading to the post office in time to mail them. My, how things have changed.
Even with all of these breakthroughs, there is still a risk in the day-to-day processes, especially in the areas of billing, coding, and documentation. After all, a computer is only as accurate as the information it can access or the information the user inputs. When it comes to billing, a system will fill in information on a claim form based on what it is given.
There are multiple areas of a CMS-1500 billing form where errors can occur, but let’s turn our focus to box 24E. This box is for diagnosis pointing, which corresponds to diagnosis box 21. With many of the software systems available today, the default information set to auto-populate this box is ABCD. This default shows the four positions available for the pointers. If this is the case, be cautious and do not assume that the software automatically makes changes when diagnosis codes go beyond the “D” position of the potential 12 spots for diagnosis available in box 21.
To paint a more precise picture, let’s say that following an examination, it was ascertained that there are six
** Today, that turnaround time is one to two weeks and payment is deposited automatically. JJ
diagnoses for the patient’s complaints. Those six codes should be listed in the order of severity on the claim form in box 21, positions A through F. In box 24, it should indicate what services were rendered to the patient on the specific date of service and relate back to the diagnoses in box 21. First list the date (24A: From/To), then the place of service (24B), procedure codes (CPT) and any modifiers (24D), diagnosis pointers (24E), charges (24F), units (24G), and rendering provider NPI (24J). If the patient has more than one service or dates of service, this information will repeat in each line of box 24.
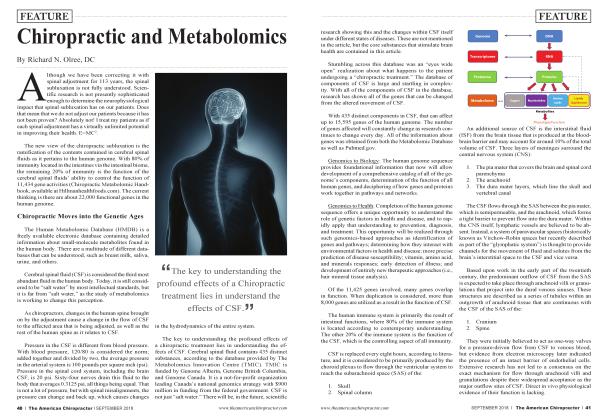
Because chiropractic deals with the spine, this example will be easiest to follow using spinal versus extra-spinal codes. Let’s say that the six diagnosis codes are as follows: (Fig. 1)
21. Diagnosis or Nature of Illness or Injury Relate A-L to service line below (24E) A. M9903 B. M544 C. M9904 D. M2170 E. M62838 F. M9905 G. H. 1. J. K. L.
Then, services in box 24 would look like this (shown with the coordinating boxes): (Fig. 2)
24. A. Date(s) of Service c D. Procedures, Services or Supplies From To TohteT SCharges Days or ID. pRendering# MM DD YY MM DD YY EMG CPT/HCPCS Modifier 061 211 18 06 i 21 i 18 11 | 98940| ABCD | 45 ! 00 123456789 06 21 18 06 21 18 11 1 98943| ABCD | 23:00 123456789 061 21: 18 06 i 21 i 18 11 | 97014| ABCD | 45 ! 00 123456789
In the example shown above, there is one line of service for a spinal adjustment, one for an extra-spinal adjustment, and the third for electric muscle stimulation. In item 24E, notice that it indicates every service was performed because of, and in direct relationship to, all of the diagnoses in positions ABCD. A closer look at the actual diagnosis codes and descriptions reveals the beginning of a big problem.
A) M99.03 - Segmental and somatic dysfunction of lumbar region
B) M54.5 - Low back pain
C) M99.04 - Segmental and somatic dysfunction of sacral region
D) M22.11 - Recurrent subluxation of patella, right knee
E) M62.831 - Muscle spasm of calf
The 98940 spinal manipulation should only relate to the first three diagnosis pointers and not the last two. Clearly, the spinal manipulation service is not for the right knee or the service to the calf The D should be removed from item 24E across from the spinal manipulation.
Observe the second line of service (98943), where the diagnosis pointer relates back to ABCD—all of the diagnoses. The conditions noted wouldn’t provide medical necessity for an extra-spinal adjustment. Only the diagnosis code in position D corresponds to the extremity. For this claim to be filed correctly, only letter D should be in box 24E for the second line of service.
Additionally, the third line of service has also defaulted to all of the diagnosis codes in item 24E. The electric muscle stimulation (97014) should be related to the muscle spasm, which also corresponds to the provider’s treatment plan in the initial visit note.
Here is how the corrected claim should look: (Fig 3)
06 21 18 06 21 18 11 | 98940| ABC | 45:00 123456789 06 21 18 06 21 18 11 1 98943| D | 23; 00 123456789 06 i 211 18 06i 21i 18 11 | 97014| E | 45i00 123456789
If more than four diagnosis codes must be reported in a line item, diagnosis pointers can be listed with a hyphen, such as A-L.
It is imperative to properly report services to third-party payers. Often, the CMS-1500 billing form is the only communication the carrier will receive that represents the provider’s intention for billing and coding. All team members should be aware of this information and billing claims should be spot-checked frequently for accuracy. Once the documentation, billing, and coding coincide, being paid properly is a snap.
Kathy Mills Chang is a certified medical compliance specialist (MCS-P), certified chiropractic professional coder (CCPC), and certified clinical chiropractic assistant (CCCA). Since 1983, she has been providing chiropractors Math reimbursement and compliance training, advice, and tools to improve the financial performance of their practices. Kathy leads a team of 30 at KMC University and is known as one of our profession's foremost experts on Medicare, documentation, and CA development.
Rhonda Hodge began her career in chiropractic in 2000. She became an account manager in the office where she had been a patient. Rhonda has extensive experience with the regulations, training, and guidelines associated with the Occupational Safety and Health Administration (OSHA). She is also very well versed in safety and loss prevention and is currently focused on compliance. Rhonda became a medical compliance specialist - physician (MCS-P) in 2012. That same year, she joined KMC University, where she has helped clients complete Medicare enrollments for their patients and written curriculum and training webinars. Rhonda has extensive experience with finances, front-desk operations, training, billing and collections, Medicare, and compliance.
Kathy or any of her team members can be reached at 855-832-6562 or info@ KMCUniversity. com
 View Full Issue
View Full Issue