A Jump Start on Geriatric Health to Conquer Alzheimer's Disease
FEATURE
WELLNESS
Alzheimer's disease is the only known killer that is on the rise.
Trish Leigh
PhD., BCN
Millions of people are affected by Alzheimer’s disease in the United States. One in three senior citizens will die from Alzheimer’s this year. People with Alzheimer’s disease, and related dementias, struggle with a decline in their ability to think, remember, and enjoy life. Not only that, but they also suffer from psychiatric disorders and over time can no longer take care of themselves in the most basic of ways from toileting to eating to moving independently.
Tens of millions of family members take care of them without being paid for their efforts. These caregivers struggle with mental health challenges, such as anxiety and depression, more than people who are taking care of loved ones who are aging well. Increases in physical pain due to the stress of caregiving are higher in these caregivers too. Many times, younger caregivers have a hereditary predisposition for Alzheimer’s disease in the first place. Thus, Alzheimer’s is not only taking a toll on those who have it, but it also is wreaking havoc on the health and wellness of their family members too.
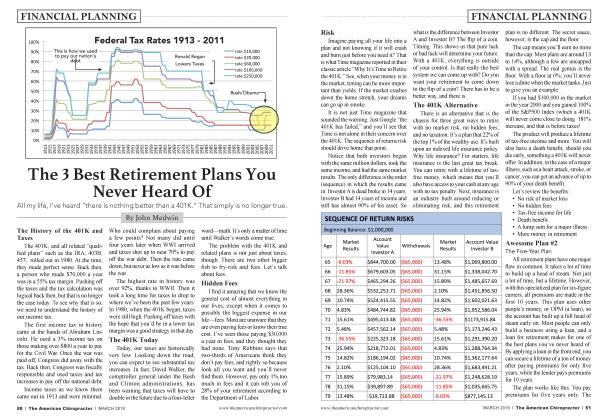
The numbers are astounding and are slated to more than double in upcoming years. This means that more than 35 million people will be at risk for a hereditary predisposition to Alzheimer’s disease and will be under a great deal of stress as they take care of their afflicted loved ones too. Alzheimer’s disease is the only known killer that is on the rise. All others, such as heart disease, breast cancer, prostate cancer, and HIV, are declining while Alzheimer’s is skyrocketing.
Shifting the Focus to Caregivers Can be the Key to Success in Conquering Alzheimer’s Disease
It may be difficult to stop the progression of Alzheimer’s in those who already have it, but the key to a societal shift in conquering this disease is helping the younger caregivers avoid it. As the incidence of Alzheimer’s disease goes up, it becomes a self-perpetuating cycle of increase due to the harm it is doing to younger caregivers. There is a way to break the cycle.
What Is Alzheimer’s and What Causes It?
Several changes occur in the structure and function of the brain to create Alzheimer’s disease. The first and most widely known change is the accumulation of tau proteins that disrupt the neurochemical flow of information between the 100 billion neurons that have 100 trillion synaptic connections in the brain. This disruption blocks neuron-neuron communication and the transport of essential nutrients to keep brain cells healthy. In turn, this causes significant amounts of inflammation and atrophy of cells. Inflammation is created as the brain tries to clear the toxic proteins and atrophy as a decreased ability to metabolize glucose happens.
These structural and functional differences make it so that the electrical speed of transmission within the brain’s neural pathways slows down. This shows up as an irregular brain pattern on quantitative electroencephalogram (qEEG), the method of measuring brain electrical performance.
The irregular brain pattern that is associated with Alzheimer’s is one of “low and slow” performance. This is indicated by low use of optimal brain processing speed, beta, and excessive use of extra slow electrical speed, delta. Essentially it is as if the person’s brain is using the “thinking brake” (delta) with great force while driving and not pressing the “thinking gas” (beta) hard enough. This results in difficulty processing information, remembering, maintaining a positive mood, and carrying out activities of daily living (ADLs).
When Does Alzheimer’s Start for a Person?
Although symptoms become apparent as a person ages, scientific studies show that the beginning of Alzheimer’s disease occurs 20 years before that. As the brain’s function begins to decline earlier in life, it selfcompensates for the changes. This enables the person to function typically for many years after the initial decline in function begins. This self-compensation has been shown to be an increase in the extra fast electrical brain speed, high beta, as measured on qEEG. This brain pattern can cause anxiety or hypervigilance throughout the person’s lifetime as the brain self-compensates. Women suffer from this brain pattern more than men do. In fact, scientific studies have shown that women are at the highest risk for Alzheimer’s and especially those who were anxious and neurotic in their 30s. The way a person uses their brain across their lifetime is proven to impact the likelihood of them developing Alzheimer’s disease. Those who are anxious, highly particular, and stressed are at highest risk.
What Can Chiropractors Do to Prevent and Remediate Alzheimer’s?
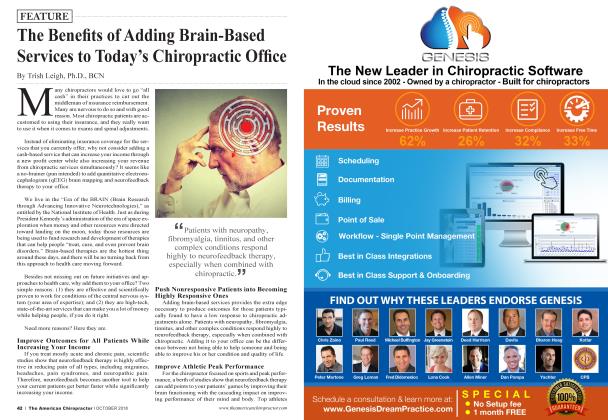
Using qEEG brain mapping, chiropractors can assist in the early detection of the irregular brain pattern that is seen in Alzheimer’s disease. If a person evidences the “low and slow” brain pattern, the compensating brain pattern of anxiety, and especially a family history of Alzheimer’s or dementia, then comprehensive chiropractic care is warranted. This care should include neurofeedback therapy for best results in addition to spinal alignment, very specific nutritional supplements to assist the Alzheimer’s brain pattern, and lifestyle changes.
Neurofeedback therapy is a treatment modality that is completely noninvasive, but it teaches the brain to improve its own performance through a learning conditioning. The brain learns to make more ideal processing speed for calm thinking and less slow and fast speed. Thus, the brain processes information at the most desired speed for optimal mental and physical performance.
Neurofeedback therapy has been proven through scientific studies to not only improve the electrical speed of the brain in patients with Alzheimer’s, but also to create sustained improvements in cognitive performance of thinking and memory. A significant decline in psychiatric symptoms was seen after a treatment program of neurofeedback therapy as well. Improving a person’s brain pattern is important, but more importantly, decreasing their symptoms and increasing their quality of life is pivotal.
In a groundbreaking scientific study, neurofeedback therapy has been proven to improve the brain at the cellular level. Researchers found that the white matter pathways in the brain—those responsible for sustained attention and cognition—improved their transmission of information through neurofeedback therapy. Additionally, the gray matter volume increased in the regions for cognition and memory after neurofeedback. Therefore, more healthy brain cells were evident following neurofeedback therapy and better working connections too. Improvements in the physical and functional nature of the brain can be the difference between disease and healthy aging.
That being stated, it is more difficult to improve the brain performance of a person who has already suffered a significant decline in physiological brain functioning and demonstrates strong dementia symptoms. It is much easier is to prevent the decline in brain performance in the first place. We know that Alzheimer’s starts in the brain earlier in life. We know that the brain can be helped more efficiently earlier in life too. Thus, Alzheimer’s can be reduced or eliminated by identifying the brain patterns in those who are at greatest risk and providing the treatment that is necessary to keep their brain healthier across their lifetime.
Dr. Trish Leigh, Ph.D., BCN has been an I educator for 20 years and operates a thriving | ⅛ :>⅛⅜¾¾ Neurofeedback practice, Leigh Brain and Spine, with her Chiropractor husband. With a proven office system in place, she is dedicated to teaching professionals how to build an effective and profitable neurofeedback practice through her 5-week online training course, Neurofeedback Experts. Program details can be found drtrishleigh.com or to talk with Dr. Leigh call 919-401-9933.
References
1. Berman, M.H. & Frederick, J.A., Efficacy of Neurofeedback for Executive and Memory Function in Dementia, Alzheimer’s and Dementia, 2009, 5(4).
2. Ghaziri, J., et al., Neurofeedback Training Induces Changes in White and Gray Matter, Clinical EEG Neuroscience, 2013, 00(0), 1-8.
3. Jack, C.R. et al., Serial PiB and MRI in Normal, Mild Cognitive Impairment and Alzheimer’s Disease: Implications for Sequence of Pathological Events in Alzheimer’s Disease. Brain, 2009; 132:1355-65, 15.
4. Johansson L. et al., Midlife Personality and Risk of Alzheimer’s Disease and Distress: A 38-year Follow-up. Neurology, 2014; 83(17): 1538-44.
5. National Institutes of Health. National Institute on Aging. What Happens to the Brain in Alzheimer’s Disease? Available at https://www.nia.nih.gov/ health/what-happens-brainalzheimers-disease. Accessed December 18, 2018.
6. Spillman B., et al., Informal Caregiving for Older Americans: An Analysis of the 2011 National Health and Aging Trends Study. Available at: https://aspe.hhs.gov/report/informal-caregivingolder-americans-analy sis-2011 -nationalstudycaregiving. Accessed December 19, 2018
 View Full Issue
View Full Issue