My Search
I recall an incident that took place over 20 years ago while I was teaching in the postgraduate department at Logan College in St. Louis, Missouri. A chiropractor studying the new technique I was teaching was inspired to begin looking at his work in a new way. After completing the introductory program, he showed me a plastic card that he had been carrying in his wallet for several years. It was permanently embossed with his “listings,” so that any chiropractor who treated him would know what to treat. This was evidence, he proclaimed, that the techniques he had been taught until then were merely focused on treating symptoms ad infinitum and not intended to resolve the underlying cause of the problem!
In over 40 years of practice, I have continuously pursued the goal of creating an evidence-based practice based on quantifiable and predictable clinical improvement. In other words, I was determined to find the Holy Grail of treatment:
1. Precisely determining the underlying structural or biomechanical cause of the problem that produced the symptoms (pain or dysfunction).
2. Providing reproducible therapeutic interventions that would produce consistent and measurable outcomes.
I knew that if I could confidently produce and consistently demonstrate positive clinical improvement, both the patient and I would know that we were on a path to recovery and resolution, rather than just temporary pain relief. Over the years, I have noted that most patients, even when they were still in some degree of discomfort, would stay with the course of treatment because they were able to directly experience objective evidence of improvements, such as improved ranges-of-motion, joint stability, and normalization of posture, structure, and neurological function.
An Unexpected Discovery
During my studies in chiropractic school, one of my earliest discoveries was that the size of a certain osseous structure on one side of the body was often larger than its counterpart on the other side (e.g., tibial plateau, distal femoral condyle, patella, femoral proximal head, and acetabulum, or the proximal epiphysis of the humerus). I first noticed this by observing radiographs and cadaver specimens. No one could explain these findings, but many years later, I encountered the scientific basis for these changes.
A Sound Scientific Basis
Over the years, I was fortunate to meet several researchers and clinicians from various fields of study (cell biology, biomedical engineering, orthopedic medicine, osteopathy, and physical medicine), who were uncovering the underlying effects of injury and biomechanical dysfunction at the cellular, molecular, and bioelectrical level. I ultimately recognized that, for any system of therapeutics to be valid, it had to be congruent with this emerging science.
“Molecules, cells, tissues, organs, and our entire bodies use ‘tensegrity' architecture to mechanically stabilize their shape and to seamlessly integrate structure and function at all size scales. Through the use of this tension-dependent building system, mechanical forces applied at the macroscale produce changes in biochemistry and gene expression within individual living cells. This structure-based system provides a mechanistic basis to explain how the application of physical therapies might influence cell and tissue physiology. ”
Donald E. Ingber, MD, PhD
The underlying structure of the body is now understood to be based on the inherent properties of the cytoskeleton and the extracellular matrix (ECM). These groundbreaking discoveries were made by orthopedic surgeon Stephen Levin, MD1, the originator of the term “biotensegrity,” cell biologist Donald Ingber, MD, PhD2, and others3. This underlying structure, which I have referred to as the “tensegrity matrix,” provides a balance between stability and mobility and explains many of the observed phenomena related to body support, movement, and response to stress and trauma, as well as the effects of therapeutic interventions.
Finally, I had a proven model for the structure of the body that appeared to explain how tissue expands with injury at the cellular and molecular levels. More recently, research from the University of California has confirmed the fact that bone enlarges with injury, just as I had observed so many years earlier. Dr. Paul Hansma and his team used the powerful Atomic Force microscope to detect the presence of certain protein structures within bone that expand with injury5, (see Figure 3). Injury to bone has also been shown to cause bioelectric changes6, which I have found to be a crucial factor when diagnosing and treating these injuries.
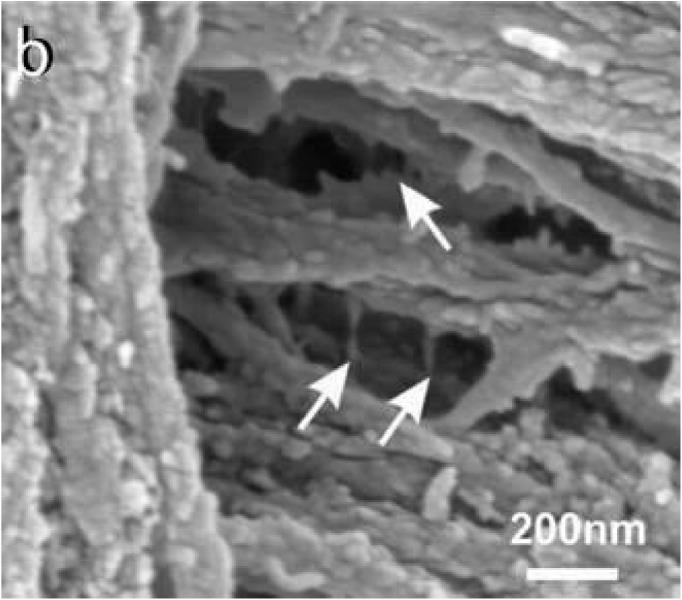 Figure 3: Microscopic Evidence of Bone with Injury, Paul Hansma Lab, University of California, Berkeley, 2005. (with permission from the author)
Figure 3: Microscopic Evidence of Bone with Injury, Paul Hansma Lab, University of California, Berkeley, 2005. (with permission from the author)
Objective Evidence of Clinical Improvement
One of the major clinical breakthroughs that my colleagues and I were able to accomplish was that bone size appeared to be restored to normal with the type of treatment we had developed. At first, we questioned these results and followed them up with precise measurements using calipers and tape measures. Inter-tester validation appeared to confirm our findings.
Several years ago, I treated a 15-year-old male hockey player who had suffered from knee pain for several months. It prevented him from playing and caused considerable pain during normal daily activities, such as climbing stairs, which he was only able to accomplish in a slow, hobbling manner. Fortunately for me, orthopedic surgeons were monitoring the size of the bones at the knee with a high degree of precision because of an underlying genetic condition. As a result, they took consistent measurements to within one-hundredth of a millimeter. They were all surprised when the femoral condyle and the tibial plateau of the left knee, which had been approximately 5 mm larger than its counterpart on the right, suddenly shrank by that amount after only a few treatments (see Figures 4 and 5). Subsequently, the young man’s parents noted that he was once again “flying up” the stairs with absolutely no pain. That case verified my contention that normalization of the shape of the bone is possible and appears to allow for the restoration of the joint space and biomechanical function, resulting in improved healing of the entire joint complex.
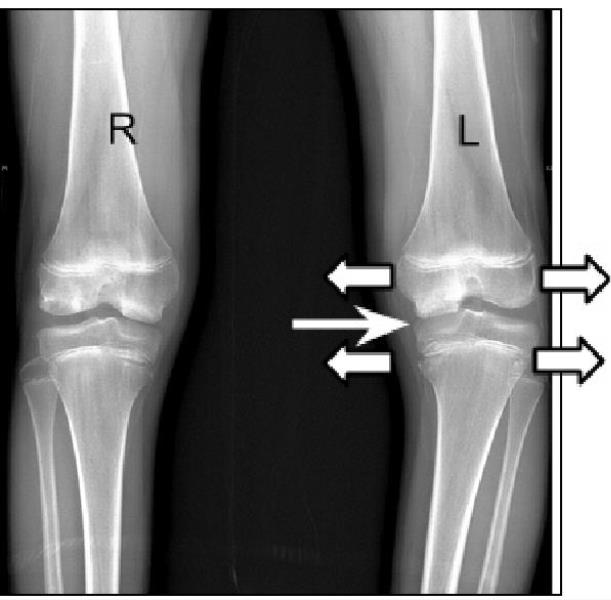 Figure 4, Pre-treatment: Femoral and tibial epiphyses enlarged, approximately 5 mm. compared to the right. *Note relative narrowing of the medial joint space.
Figure 4, Pre-treatment: Femoral and tibial epiphyses enlarged, approximately 5 mm. compared to the right. *Note relative narrowing of the medial joint space.
Subluxation: A Case of Mistaken Identity?
The subluxation theory and the idea that bones “go out of place” have long been questioned. However, I believe that the entire premise may simply be a matter of mistaken identity. By this, I mean that the palpatory impression of “misaligned vertebra” may result from enlargement of part of the vertebral segment (see Figure 6, below).
The fact that many patients achieve benefit through chiropractic adjustment may be due to its influence on the actual structure of the osseous enlargement, albeit inadvertently, on the part of the practitioner. I now believe that if practitioners were made aware of the fact that injury actually alters the shape and size of bone in the spine and throughout the body, they would be eager to apply methods that would more precisely target these areas and thus achieve even better results.
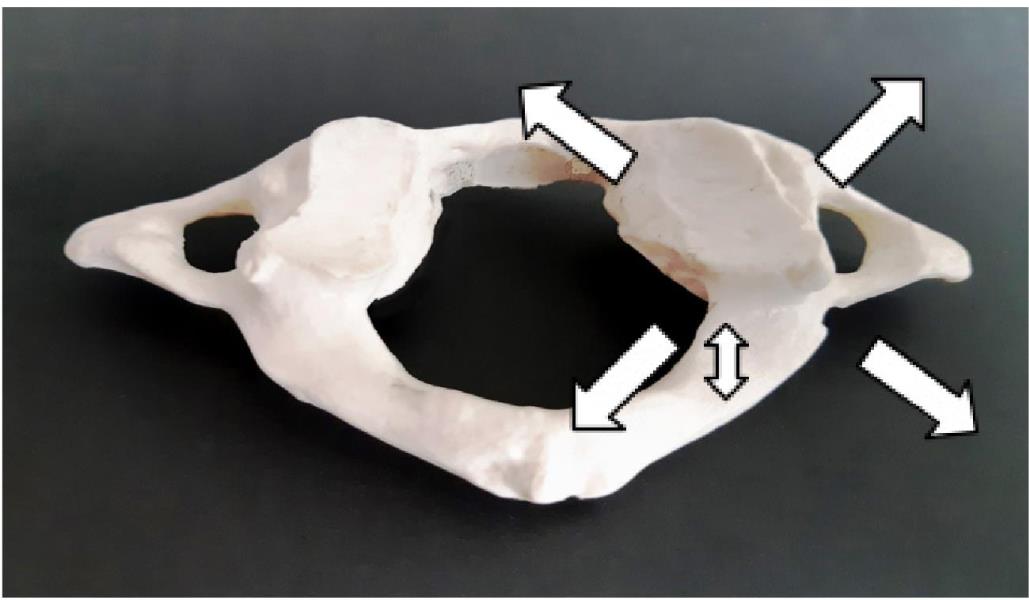 Figure 6: Model of C1, cast from a real skeletal specimen. Note the enlargement of the right articular process and the spinal canal, which measured 2mm larger in every dimension
Figure 6: Model of C1, cast from a real skeletal specimen. Note the enlargement of the right articular process and the spinal canal, which measured 2mm larger in every dimension
The Evolution of Chiropractic
Through a combination of relentless questioning and evaluation of measurable, objective changes in my own practice and those of my students and colleagues, we gradually evolved a method to identify and resolve many of the structural effects of injury and thus improve our clinical outcomes. Over the years, this protocol has been recognized by a growing number of chiropractors, as well as clinicians and researchers from various fields. I have been gratified to note that many of them were able to reproduce the same measurable outcomes, which I observed.
My goal has always been to develop techniques that chiropractors can adopt to provide profound, lasting solutions for many of the painful and limiting conditions afflicting the public. By integrating the latest developments in cellular biology, molecular biomechanics, and bioelectricity, I am convinced that we can improve upon the care we already provide and evolve even further as a truly evidence-based profession. I believe that this will allow chiropractic to take its rightful role in the healthcare industry as a leader in the field of physical medicine.
About the Author
Dr. George Roth has been practicing as a chiropractor and a naturopathic physician for 40 years. He has taught at chiropractic, naturopathic, medical, osteopathic, physical therapy, and medical schools throughout North America. He is the co-author, with Kerry D'Ambrogio PT, of Positional Release Therapy (Elsevier, 1997), and the author of The Matrix Repatterning Program for Pain Relief (New Harbinger, 2005). His work is also featured in the Brain's Way of Healing, by Dr. Norman Doidge (Penguin, 2016). For more information, visit: www.matrixforpractitioners.com.
References:
1. The Importance of Soft Tissues for Structural Support of the Body, SMLevin, In: Positional Release Therapy: Assessment & Treatment of Musculoskeletal Dysfunction, K D’Ambrogio & GB Roth, Mosby-Elsevier, St. Louis, 1997.
2. Ingber DE, The Architecture of Life, Scientific American, Vol. 1, 1998.
3. The Extracellular Matrix and Ground Regulation, Basis for a Holistic Biological Medicine, A Pischinger, North Atlantic Books, Berkley, 2007.
4. Energy Medicine, The Scientific Basis, JL Oschman. Churchill Livingstone, New York, 2001.
5. Fantner GE, Hassenkam T, Kindt JH, Weaver JC, BirkedalH, Pechenik L, Cutroni J A, Cidade GA, Stucky GD, Morse DE, Hansma PK, Sacrificial bonds and hidden length dissipate energy as mineralized fibrils separate during bone fracture, Nat Mater. 2005 Aug;4(8):612-6. Epub 2005 Jul 17.
6. Chakkalakal DA, Mechanoelectric transduction in bone. J Mater Res], 1989;4: 1034-1046.
 View Full Issue
View Full Issue