Surprising Observations
As a chiropractic intern, I noticed something that seemed to be a mystery to my instructors in the radiology department. While studying radiographic images of hips, shoulders, and knees, I often observed that an epiphysis (the end of a long bone) on one side of the body was often enlarged when compared to its counterpart on the other side. No one seemed to have an explanation. Almost 30 years later, these observations were finally validated by independent research. I contend that these bone changes are crucial to our understanding of the structural basis of injury and its implications for therapeutic intervention.
What Happens to Bone with Injury?
Objective evidence from the University of California published in 2005, revealed by the powerful Atomic Force Microscope (AFM) under the direction of physicist Dr. Paul Hansma,1 has clarified the structural effects of injury within the bone, resulting in persisting enlargement (See Figure 1).
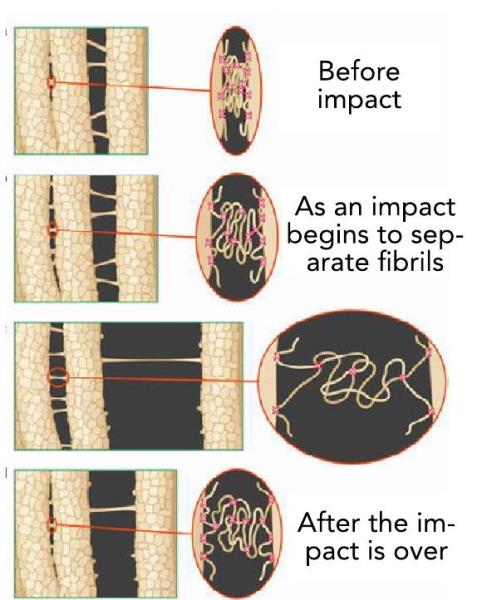 Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkeley, 2005.
Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkeley, 2005.
Putting the Puzzle Pieces Together
Over the years, I have explored a wide range of approaches within the field of structural therapy. Each technique provided a theoretical framework to support its tenets, but, to my frustration, none of them appeared to agree with each other. I knew that something was missing.
For the past 40 years, I have been on a quest to achieve more consistent, objective, and measurable results with my own practice. To achieve that, I felt there had to be a universal principle, which would explain the underlying structure of the body and its response to injury. Eventually, my search led me to explore developments in the fields of cellular and molecular biology. Emerging science regarding cellular/molecular structure, and the developing field of electro-biology, inspired me to develop a form of therapy consistent with those scientific principles. The result is a treatment system that appears to be congruent with those scientific principles, which I have taught to practitioners from around the world for almost three decades.
The Molecular/Cellular Basis of Injury
In 1992, I was fortunate to encounter Dr. Stephen Levin, a brilliant orthopedic surgeon who was lecturing on the importance of the interconnected framework of tissue as reflected in the cellular structure, which he refers to as biotensegrity.2 Cellular research conducted by Donald Ingber, MD, PhD, has since established that all living cells consist of a molecular/protein framework referred to as the cytoskeleton (See Figure 2).3 In addition, the cytoskeleton of each cell is linked to adjacent cells via the extracellular matrix (ECM), forming a continuous fabric, which I refer to as the biotensegrity matrix. It provides mechanical and electrical continuity throughout the body, which is essential to the maintenance of optimal cellular health and function. 4
When an injury occurs because of life’s unforeseen events, such as strains, falls, sports injuries, or motor vehicle collisions, physics teaches us that mechanical energy is absorbed by the densest structures of the body, namely bone and the fascia associated with certain visceral structures. Water is the densest substance in the body, so an impact injury can be absorbed by the fluid-filled compartments of the body, namely the trunk and the cranium. This often results in internal injuries to the liver, kidneys, spleen, or heart, as well as concussion affecting the fluid contents of the cranium, including the brain.
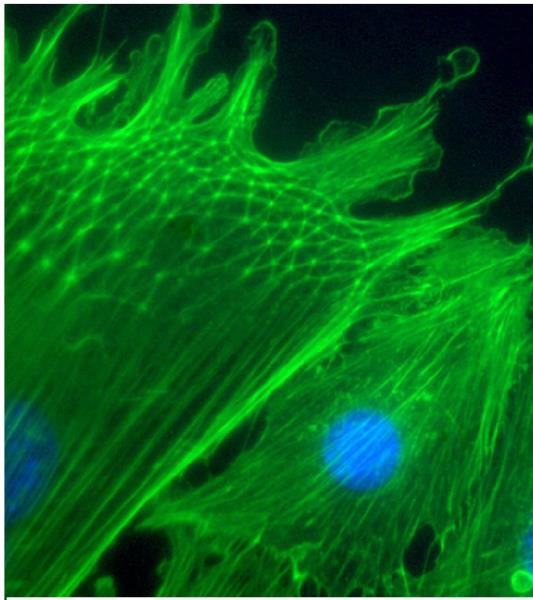 Figure 2: High-powered microscopy reveals the protein framework within the cell (cytoskeleton), which determines its structural properties and how it may respond to injury. Photo courtesy of Donald Ingber, MD, PhD.
Figure 2: High-powered microscopy reveals the protein framework within the cell (cytoskeleton), which determines its structural properties and how it may respond to injury. Photo courtesy of Donald Ingber, MD, PhD.
Thus, injury (impact or strain) is transferred to the densest components of the body, which, in turn, leads to the expansion of the molecular structure within the cell (cytoskeleton). It has been demonstrated that when cells expand in that way, they become rigid, and their electrical properties are altered.5,6 This combination of deformed tissue structure and electrical disruption has far-reaching clinical effects, causing a wide range of symptoms. This molecular/cellular response to injury is also consistent with the expansion seen in injured bone, as observed by Dr. Hansma’s team of researchers. Dr. Levin also wrote a detailed paper about the structural properties of bone as they relate to the biomechanics of the entire body. 7
Quality skeletons cast from a real specimen will allow you to verify many of these same discrepancies. For example, you may be able to notice these differences in the spine (width, depth, and height of the vertebral body, articular processes, and lamina or transverse processes). Figure 3 illustrates these differences in the size of the articular processes of Cl. On palpation, these areas of enlargement may be easily mistaken for a relative rotation or translation of the vertebral segment.
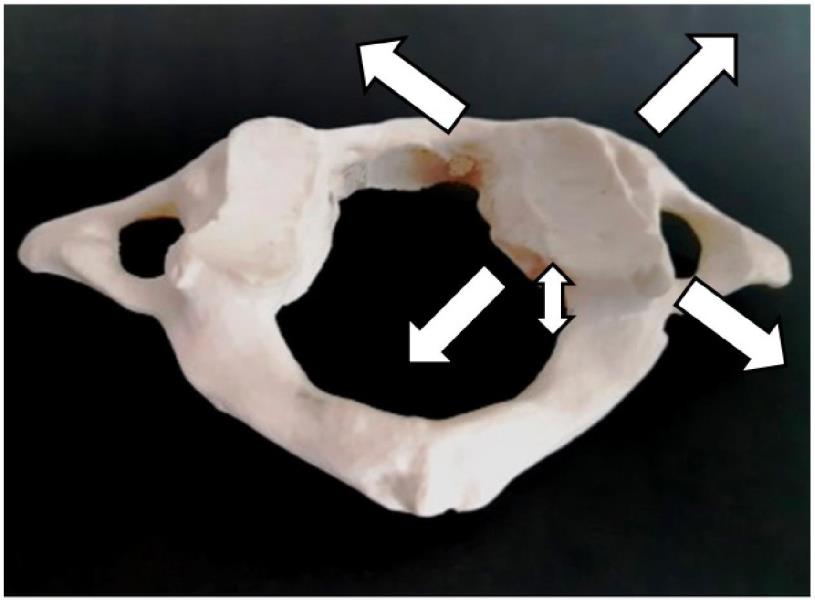 Figure 3: Model of C1, cast from a real skeletal specimen. Note the enlargement of the right articular process and the spinal canal, which measured 2 mm larger in every dimension.
Figure 3: Model of C1, cast from a real skeletal specimen. Note the enlargement of the right articular process and the spinal canal, which measured 2 mm larger in every dimension.
Case Study
Allie* is a teenage girl who struggled her entire life with a debilitating structural bone condition. Her issues began at approximately one year of age when she broke her right tibia near the distal growth plate. The tibia did not grow normally after that injury, causing a leg-length discrepancy of 4 cm by the age of nine. Ultimately, she was diagnosed with a serious bone disorder called polycystic fibrous dysplasia.

Figure 4: Pretreatment anterior, March 2017
 Figure 5: Posttreatment anterior, July 2017
Figure 5: Posttreatment anterior, July 2017
At age nine, she had a significant surgery to lengthen the affected leg. One year after this surgery, while recovering in an air-cast, she broke her tibia again. Despite an endless array of further invasive surgeries including the insertion of a Fassier-Duval rod, medications, and the use of a bone stimulator, the problems persisted, and she was told that her leg would continue to deteriorate. By the time she was 13, Allie was suffering daily from pain and often required the use of assistive devices to walk.
With the news that her condition would only worsen, her mother sought something different in hopes of relieving some of the pain. She found a practitioner trained to provide treatment to the bone structure of the body. X-rays were taken at the surgeon’s office before the treatment plan began. Four months later, after 6 treatments, new X-rays were taken that revealed something no one had expected. The images showed new healthy bone (Figures 4 through 8). This was the only type of treatment she received during this period.
Because of these treatments, Allie experienced significant pain reduction and was able to walk comfortably without assistance. To date, she is virtually pain-free. As an update, her doctors were ultimately able to remove the metal rod, which had been protruding at one end and caused irritation because her bone had healed to such a significant extent.
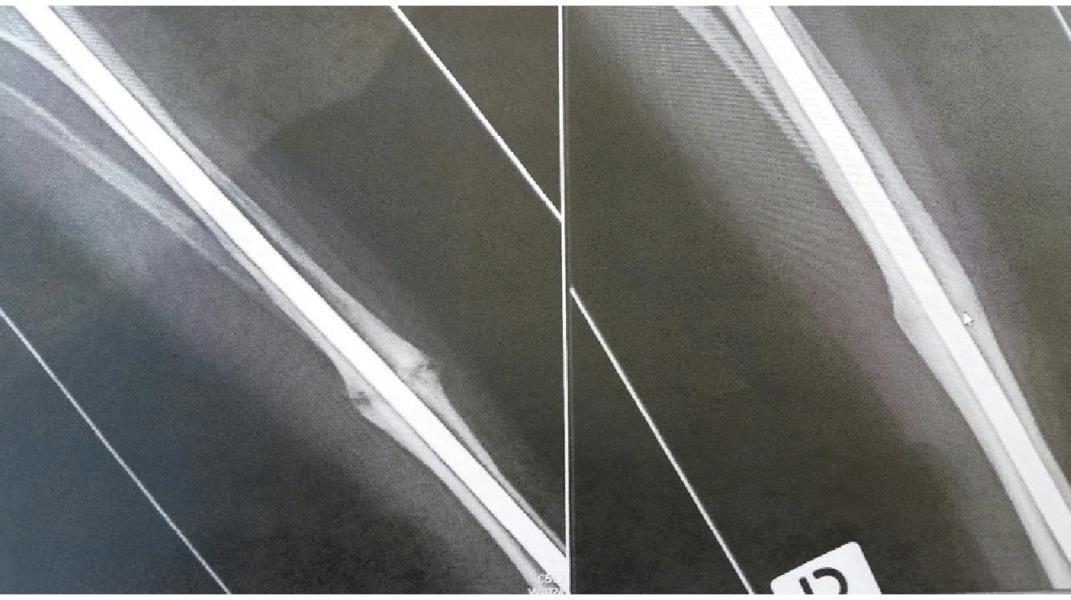 Figure 6: Pre and posttreatment anterior (detail)
Figure 6: Pre and posttreatment anterior (detail)
Prior to receiving this type of treatment, the underlying injuries were not being addressed, even though Allie was provided with the best care conventional medicine had to offer. I contend that her injuries resulted in cellular damage within the bone. Allie’s case study provides objective, radiographic evidence of tissue improvement using a specifically targeted treatment protocol directed to these tissues. By correcting the underlying issues that prevented her tibia from healing, Allie got her life back when all else had failed.
*Note: Allie is a pseudonym used to protect the privacy of this patient.
Note: In a previous article, I provided evidence of a measurable reduction in bone size, related to the distal femoral epiphysis and the proximal tibial epiphysis (“Is it Time for Chiropractic to Evolve?” December 2019).
 Figure 7: Pretreatment lateral, March 2017
Figure 7: Pretreatment lateral, March 2017
 Figure 8: Posttreatment lateral, July 2017
Figure 8: Posttreatment lateral, July 2017
Summary
The basic approach with this type of osseous protocol is to determine the precise location of tissue injury (primary restrictions) using the now established evidence that these injuries create measurable structural changes to bone and a disruption in the generation or conduction of electrical current. Treatment consists of gentle manual pressure, along with a biocompatible magnetic field to induce a piezoelectric (pressure-induced electrical current) influence, thus normalizing the electrical and mechanical properties of tissue at the injury site.8
Many chiropractors trained in the application of these precise assessment and treatment protocols have produced a significant body of clinical evidence demonstrating improvement in osseous size and shape. Importantly, these changes have been associated with measurably positive orthopedic, neurological, and physiological outcomes. This form of treatment has also been recognized as an important intervention in the treatment of concussion and certain other forms of traumatic brain injury (TBI).9
While developing this form of treatment, I attempted to take into account the scientific discoveries regarding how the body is constructed and how it responds to injury at the most fundamental level. Based on almost three decades of clinical experience and reports from practitioners around the world who have learned these methods, I believe it is possible to restore normal bone structure and other related tissue injuries to provide pain relief and improved quality of life for many of our patients.
Dr. George Roth is a graduate of the University of Toronto, Canadian Memorial Chiropractic College, and the Ontario College of Naturopathic Medicine. He also has studied osteopathic medicine at Doctors' Hospital North, Columbus, Ohio. He is the developer of Matrix Repatterning and is the director of education at the Matrix Institute in Toronto. Dr. Roth has presented seminars at numerous hospitals and university-based symposia throughout North America. He coauthored Positional Release Therapy (Elsevier, 1997) with Kerry D'Ambrogio, PT, and is the author of The Matrix Repatterning Program for Pain Relief (New Harbinger, 2005). His work is also featured in The Brain's Way of Healing by Dr. Norman Doidge (Penguin, 2016).
References:
1. Fcintner GE, Hcissenkcim T, Kindt JH, Weaver JC, Birkedal H, PechenikL, Cutroni JA, Cidade GA, Stucky GD, Morse DE, Hansma PK. Sacrificial bonds and hidden length dissipate energy as mineralized fibrils separate during bone fracture, Nat Mater 2005 Aug; 4(8): 6126. Epub 2005 Jul 17.
2. The Importance of Soft Tissues for Structured Support of the Body, SM Levin, In: Positional Release Therapy: Assessment & Treatment of Musculoskeletal Dysfunction, K D Ambrogio & GB Roth, Mosby-Elsevier, St. Louis, 1997.
3. Ingber DE. The Architecture of Life, Scientific American, Vol. 1, 1998.
4. Pischinger A. The Extracellular Matrix and Ground Regulation, Basis for a Holistic Biological Medicine, North Atlantic Books, Berkley, 2007.
5. MacGuintie LA. Streaming and piezoelectric potentials in connective tissues, In: Blank M (ed) Electromagnetic fields: biological interactions and mechanisms. Advances in Chemistry Series 250. American Chemical Society, Washington DC, ch. 8, pp 125-142, 1995.
6. Chakkalakal. DA. Mechanoelectric transduction in bone. J Mater Res. 1989:4: 1034-1046.
7. Bone is Fascia, SM Levin, In: Everything Moves: How biotensegrity informs human movement, Lowell de Soldrzano, S., Handspring, 2021.
8. Roth GB. The Matrix Repcitterning Program for Pain Relief, New Harbinger Publications, Oakland, CA, 2005.
9. Doidge, N. The Brain's Way of Healing, Penguin Books, New York, 2016.
 View Full Issue
View Full Issue