The Missing Link
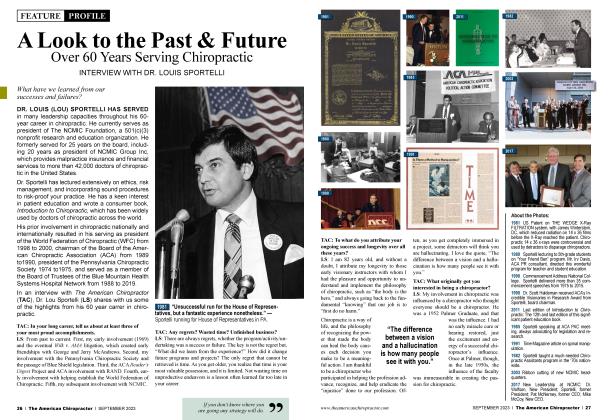
FEATURE
DOCUMENTATION
Gregg Friedman, DC
Gregg Friedman is a second-generation chiropractor who has been practicing since 1987. He has been teaching documentation and coding at the post-graduate levelfor more than 2 0years and consults with chiropractors, insurance companies and attorneys. You may contact him at [email protected].
Let’s keep talking about who makes the rules for documentation, i.e., Centers for Medicare and Medicaid Services (CMS).
I know what you’re thinking. “I don’t treat many Medicare patients, so this doesn’t apply to me.” Not so fast.
Don’t think of CMS as Medicare. Instead, think of them as “the Feds.” They create the rules for everyone in health care, regardless of who pays for the services. The good news, though, is that if you follow these rules, it will work for all of your active patients.
First, There Was Pain
In my last article, I talked about the first thing they want from us, which is to assess pain for each condition and on every visit. So now, let’s talk about the second thing.
The Second Thing
CMS requires our documentation to include a “functional outcome assessment using a standardized functional outcome assessment tool on the date of the encounter and documentation of a care plan based on identified functional outcome deficiencies on the date of the identified deficiencies.” To make this a bit easier to digest, they want us to use functional outcome questionnaires. “Functional questionnaires seek to directly quantify symptoms, function, and behavior, rather than draw inferences from relevant physiological tests.”
CMS also states that clinicians should use validated self-report questionnaires/ tools useful for identifying a patient’s baseline status relative to pain, function, and disability and for monitoring a change in a patient’s status throughout the course of treatment. Many will argue that these patient-reported outcome tools (PROMs) are subjective since the patient is answering the questions. Amazingly, there’s been some debate over this for at least 30 years; as long as the questionnaires are valid and reliable, they can be considered objective. Regardless of if they’re subjective or objective, are the questionnaires valid and reliable?
How Often?
CMS wants us to have the patient complete a functional outcome questionnaire for each complaint we’re treating on the initial visit and then every 30 days or sooner. Our care plan should include measurable treatment goals for each condition based on the scores on the functional outcome questionnaires. Other guidelines want us to reevaluate (with functional outcome questionnaires for each condition) at the mid-point of the trial, which is after two weeks or six visits, whichever comes first.
One problem I’ve seen is that some questionnaires are too complicated or time-consuming, and patients hate filling them out. The most despised ones include the Revised Oswestry Low Back Disability Questionnaire and the Neck Disability Index. While each only has 10 questions, each question has six different options, so patients have to read 60 different options and select an answer for each. There are a number of functional outcome questionnaires we can use that are much easier and faster for patients to complete.
The Key to Excellent Documentation
When you put this all together, the key to great documentation is to show how your patients’ conditions are responding to your treatment. Since chiropractic is exceptional at getting great outcomes, this is perfect for us. We must follow a few requirements, though.
We need to track the patient’s progress specifically for each condition we are treating.
We need to track the patient’s progress measurably.
We need to track the patient’s progress functionally.
All we’ve got to do is track the intensity and frequency of each condition on every visit and have the patient fill out the functional outcome questionnaire for each condition on the first visit and then every thirty days or sooner thereafter.
By documenting the measurable and functional progress of each patient and each condition, we will effectively satisfy every set of guidelines thrown at us. As someone who has reviewed chiropractic records for many years, I’m not concerned with how you actually treat the patient. You want to adjust only? Fine by me. You want to use modalities? Go for it. You want to focus on rehab exercises with your patients? I’m good with that.
Just Show Me the Progress
Progress is really all that anyone is looking for in your records. Is your patient experiencing measurable and functional improvement for each condition you treat? Great. If, at the mid-point of the thirty-day trial, the patient is showing measurable and functional improvement, but the numbers are not yet normal or plateaued, you are justified to continue treating the patient for the rest of the trial (another two weeks or six visits, whichever comes first). Then, do it again. And again.
 View Full Issue
View Full Issue