Self-Management and Minimizing Catastrophizing of Chronic Low Back Pain Versus Chiropractic Care
By Mark Studin DC, FPSC, FASBE(C), DAAPM
“Catastrophizing is a cognitive distortion that prompts people to jump to the worst possible conclusion, usually with very limited information or objective reasons to despair. When a situation is upsetting but not necessarily catastrophic, they still feel like they are in the midst of a crisis.” — Psychology Today1
Low back pain remains the leading cause of years lived with disability globally since 1990, with the number of incidents increasing since 2019. The ages peaked at 45 to 54 years for both sexes and peaked at 80 to 84. The highest incidence globally is in North America.
When managing chronic low back pain (CLBP), much of the literature supports lifestyle modification, diet, education, physical therapy, pharmacological treatments, psychotherapy, and surgery.2 Many clinical guidelines are unfortunately too similar. Despite those guidelines for managing low back pain, the gap between the evidence and practice is pervasive.3
Scholz et al.4 reported that self-management interventions might convey ways to make life easier despite the pain, which may be reflected in a more pronounced improvement in pain-related functioning compared with pain intensity. With methods like cognitive behavioral therapy, coaching, motivation, and relaxation, “psychosocial factors” of pain influence of higher pain severity on the emotional state or the dysfunctional cycle between increased catastrophizing and greater pain severity might be treated specifically, which play an important role in the development and maintenance of chronic pain. It is also felt that digital self-management interventions are expected to reduce pain-related thoughts in patients and manage feelings of helplessness if they are in pain. Also, recent evidence suggests that pain catastrophizing is a key outcome in patients with back pain, and that it is worth investigating treatment programs specifically tailored to reduce catastrophizing.5
The preference for self-management and cognitive behavioral therapy was evidenced recently with one of my patients in a veteran’s administration hospital in Philadelphia. The radiologist misdiagnosed a significant disc extrusion, and a healthy, rugged 40-year-old female military police officer was treated with a combination of physical therapy and opioids that failed in part due to a missed diagnosis and mismanagement. This was followed by neurological and pain management intervention, which also mismanaged the patient by not looking at the images and relying on other doctors’ reports. When medicine failed, she was placed in cognitive behavioral training to help her minimize the catastrophizing of the pain. It failed. According to addiction medical (ADM) specialists,6 unless you work to correct the underlying cause of the pain, the likelihood of disparate treatments is unlikely to help, leading to escalating addictive drugs to tolerate the pain.
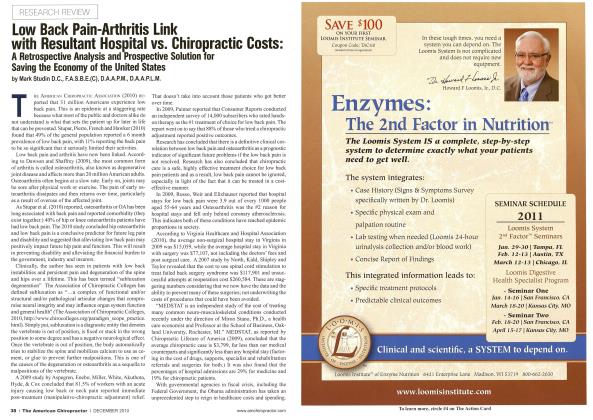
As mentioned earlier, Foster et al.3 reported that providers are not following the evidence in the literature regarding outcomes. According to Blanchette et al.,7 chiropractic realizes 313% better outcomes in secondary disability than physical therapy if the first provider for care and 239% better outcomes for primary disability. Ndetan et al.8 reported that over 96% of survey respondents with spine-related problems said the use of chiropractic manipulation stated that the therapy helped them with their condition, with approximately 46% increased odds that it helped compared to osteopathic manipulation. Compare these statistics to medicine, which persists in diagnosing 90 to 95% as nonspecific low back and significant evidence of a perpetual failed care path.9
Whedon et al.10 reported the average annual charges per person for filling opioid prescriptions were 74% lower among chiropractic recipients than other therapies. They also reported the adjusted likelihood of filling a prescription opioid analgesic was 55% lower for recipients of chiropractic services provided by a doctor of chiropractic compared with other therapies.
A prominent, well-published neurosurgeon who treats patients globally considers the primary referral for nonspecific (no fracture, tumor, infection, or operable herniation) back pain a combination of bed rest, drugs, and physical therapy, despite being shown this evidence as recently as January 2024. The surgeon went out of their way to say, “I know the research, and you won’t be happy, but that is my best recommendation.” This pervasive attitude and actions are why low back pain is a worldwide epidemic and is increasing in North America.
The “flip side of the coin” is chiropractors who ignore ancillary treatments to support chiropractic care. Adding bed rest, lifestyle changes, exercise, and cognitive therapies could help patients function better while they are getting better, as evidenced by the statistics previously cited. The title of this article — “Self-Management and Minimizing Catastrophizing of Chronic Low Back Pain Versus Chiropractic Care” — should read “Self-Management and Minimizing Catastrophizing of Chronic Low Back Pain with Chiropractic Care as the Primary Treatment.”
This is about resolving a global epidemic and is in the public interest.
About the Author
Dr. Mark Studin has been practicing chiropractic for 43 years. He is an adjunct professor at the University of Bridgeport, School of Chiropractic, Cleveland University Kansas City College of Chiropractic and the State University of New York at Buffalo, Jacobs School of Medicine and Biomedical Sciences, Family Medicine Department. Dr. Studin consults doctors nationally on increasing utilization in personal injury based on clinical excellence and compliance. He can be reached at [email protected] or 631-786-4253.
References
PsychologyToday.com [Internet]. Psychology Today. [cited 2024 Feb]. Available from: https://www.psychologytoday.co...
Chen S, Chen M, Wu X, Lin S, Tao C, Cao H, Shao Z, Xiao G. Global, regional and national burden of low back pain 1990-2019: a systematic analysis of the global burden of disease study 2019. J Orthop Translat. 2021 Sep 10;32:49-58. doi: 10.1016/j.jot.2021.07.005. PMID: 34934626; PMCID: PMC8639804.
Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG. Lancet low back pain series working group: Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018 Jun 9;391(10137):2368-2383. doi: 10.1016/S0140-6736(18)30489-6. Epub 2018 Mar 21. PMID: 29573872.
Scholz C, Schmigalle P, Plessen CY, Liegl G, Vajkoczy P, Prasser F, Rose M, Obbarius A. The effect of self-management techniques on relevant outcomes in chronic low back pain: a systematic review and meta-analysis. Eur J Pain. 2023 Dec 9. doi: 10.1002/ejp.2221. Epub ahead of print. PMID: 38071425.
Darnall BD, Krishnamurthy P, Tsuei J, Minor JD. Self-administered skills-based virtual reality intervention for chronic pain: randomized controlled pilot study. JMIR Form Res. 2020 Jul 7;4(7):e17293. doi: 10.2196/17293. PMID: 32374272; PMCID: PMC7381022.
Studin M, Coppola P. Addictionology, back pain and chiropractic. Dynamic Chiropractor. 2023;41(2):53-55. Available from https://dynamicchiropractic.co...
Blanchette MA, Rivard M, Dionne CE, Hogg-Johnson S, Steenstra I. Association between the type of first healthcare provider and the duration of financial compensation for occupational back pain. J Occup Rehabil. 2017 Sep;27(3):382-392. doi: 10.1007/s10926-016-9667-9. PMID: 27638518.
Ndetan H, Hawk C, Evans W, Tanue T, Singh K. Chiropractic care for spine conditions: analysis of national health interview survey. J Health Care and Research. 2020 Jul 25;1(2):105-18.
MayoClinic.org [Internet]. Mayo Clinic. c2023 [cited 2024 Feb]. Available from: https://www.mayoclinic.org/diseases-conditions/back-pain/diagnosis-treatment/drc-20369911
Whedon JM, Uptmor S, Toler AWJ, Bezdjian S, MacKenzie TA, Kazal LA Jr. Association between chiropractic care and use of prescription opioids among older medicare beneficiaries with spinal pain: a retrospective observational study. Chiropr Man Therap. 2022 Jan 31;30(1):5. doi: 10.1186/s12998-022-00415-7. PMID: 35101064; PMCID: PMC8802278
 View Full Issue
View Full Issue