CHRONIC PAIN AFFECTS OVER 50 MILLION adults in the United States, significantly impairing quality of life and posing a substantial burden on healthcare systems. As the opioid crisis underscores the urgent need for non-pharmacologic interventions, chiropractic care has emerged as a critical component in conservative pain management. This article explores the role of chiropractic assessment, spinal manipulation, functional rehabilitation, and patient education in combating chronic pain, focusing on evidence-based strategies and current clinical guidelines.
Chronic pain, defined as pain lasting longer than three months, is among the most prevalent and costly health issues globally. It transcends mere physical discomfort, often leading to depression, anxiety, reduced mobility, and diminished quality of life.1 Although pharmacologic interventions remain widespread, growing concerns about side effects, dependency, and long-term efficacy have sparked interest in integrative and non-drug therapies.
“Chronic pain, defined as pain lasting longer than three months, is among the most prevalent and costly health issues globally.”
With its biomechanical and neuromusculoskeletal focus, chiropractic care offers a comprehensive approach to chronic pain rooted in functional improvement, structural correction, and patient empowerment. Chiropractors are uniquely positioned to address the multifactorial nature of chronic pain by targeting both its physiological and behavioral components.
Chronic pain is not merely a continuation of acute pain; it often represents a maladaptive neurological response involving central sensitization. This phenomenon is characterized by an amplified perception of pain, even without ongoing tissue damage.2 Contributing factors include inflammation, structural dysfunction, psychosocial stress, deconditioning, and disrupted proprioception.
Traditional biomedical models often fail to effectively treat chronic pain because they focus on isolated symptoms rather than system-wide dysfunction. Chiropractic care aligns with the biopsychosocial model, which recognizes the interplay between physical, psychological, and social factors in pain expression.
One of the most researched chiropractic interventions is spinal manipulative therapy (SMT). SMT involves applying controlled, high-velocity, low-amplitude thrusts to spinal joints to restore mobility, reduce nociceptive input, and improve neuromuscular function.
Low back pain alone is the leading cause of disability among high and middle-income countries and continues to grow among lower-income countries.3 Low back pain in 2015 alone was the cause for over 60 million years lived in disability.3 This is a 54% increase since 1990.3 These statistics should lead chiropractic into the battle against chronic pain.
A 2021 meta-analysis published in BMJ found SMT to be as effective as recommended interventions (e.g., exercise, physical therapy, NSAIDs) for reducing pain and improving function in chronic low back pain patients.4 Similarly, a 2020 Cochrane review concluded that SMT produced moderate improvements in pain and disability compared to placebo or sham interventions.5
Mechanistically, SMT may work by reducing central sensitization, improving segmental mobility, and enhancing proprioceptive signaling. Neuroimaging studies have shown changes in brain activity associated with manual therapy, further supporting its central effects.6
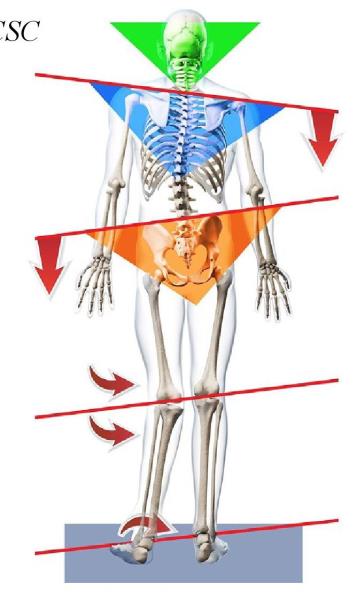
Postural imbalances and kinetic chain dysfunctions often underlie or perpetuate chronic pain. Excessive thoracic kyphosis, forward head posture, leg length discrepancies, and flat feet can all contribute to abnormal loading patterns and compensatory motor behaviors.7
Chiropractors use tools such as digital posture analysis, motion palpation, gait evaluation, and surface electromyography (sEMG) to identify mechanical contributors to pain. Correcting postural misalignments through adjustments, custom flexible orthotics, custom cervical pillows, and targeted exercise can help redistribute mechanical stress, restore proper joint motion, and reduce nociceptive input.
A 2023 study in the Journal of Orthopaedic Science demonstrated that postural realignment significantly improved pain and disability among patients with chronic musculoskeletal pain7. Chiropractic care excels in recognizing these often-overlooked drivers of pain and crafting structural solutions.
Although manual therapy offers immediate relief, long-term management of chronic pain often hinges on restoring proper movement patterns and neuromuscular control. Chiropractors integrate therapeutic exercises, proprioceptive training, and neuromuscular reeducation to rebuild functional capacity and reduce reinjury risk.
Core stabilization, for instance, is a common intervention in patients with low back pain. Exercises targeting the transverse abdominis, multifidus, and diaphragm have enhanced spinal stability and reduced recurrence rates.8
In addition, therapeutic movement approaches such as McGill stabilization, DNS (Dynamic Neuromuscular Stabilization), and active care protocols emphasize motor control and endurance over brute strength. These methods are particularly effective in reducing pain-related fear-avoidant behaviors and rebuilding confidence in movement.
One of the most underappreciated tools in combating chronic pain is education. Chronic pain alters how patients think and behave. Many develop catastrophizing beliefs, avoidance behaviors, and a reliance on passive treatments. Chiropractors are in a key position to help patients understand their condition, dispel fear, and reinforce active coping strategies.
The Clinical Practice Guidelines from the American College of Physicians recommend nonpharmacological, selfcare-focused approaches—like those provided by chiropractic practitioners—as first-line treatments for chronic pain.9
Explaining the nature of chronic pain, introducing graded exposure to feared movements, and reinforcing lifestyle change (e.g., sleep hygiene, physical activity, mindfulness) are powerful tools that enhance treatment outcomes.
Many chiropractic clinics offer complementary modalities such as:
• Pulsed Electromagnetic Field (PEMF) Therapy: Enhances cellular repair and reduces infl aimnation. 10
• Red Light Therapy: Stimulates mitochondrial activity and reduces musculoskeletal pain.11
• Instrument-Assisted Soft Tissue Mobilization (IASTM): Breaks down scar tissue and improves tissue perfusion.
• Custom Flexible Orthotics: Correct lower kinetic chain dysfunctions contributing to pain patterns. Supporting the foundation of our bodies will establish a superior biomechanical advantage during the healing phase of injury.
• Custom Pillow: More research has been done on the importance of quality sleep and rest in facilitating recovery and expediting healing. Ergonomic sleep positions and the importance of quality support during sleep should be emphasized to the patient.
These adjuncts offer a multimodal approach to pain management, helping to address complex, chronic pain presentations from multiple angles.
Chronic pain remains a major clinical and societal challenge. Chiropractic care offers an evidence-informed, patient-centered, and non-pharmacologic approach that addresses pain’s mechanical, neurological, and behavioral aspects. Chiropractors empower patients to regain function, reduce suffering, and improve quality of life through spinal manipulation, postural correction, movement rehabilitation, and patient education.
As healthcare systems continue to seek effective alternatives to opioids and surgery, chiropractic’s role in chronic pain management is more relevant than ever. By integrating clinical expertise with current research, chiropractors can deliver compassionate and cost-effective care to combat one of our time’s most persistent health burdens.
Dr. Christine Foss is the Director of the Certified Chiropractic Sports Physician Program for Northeast Chiropractic College and Director of Education for the International Certification of Sports Chiropractic. She was named the 2020 American Chiropractic Association Sports Council Chiropractor of the Year and was the 2023 International Federation of Sports Chiropractic Educator of the Year. She is currently the director and lead instructor of the Northeast Chiropractic College, “Certified Chiropractic Sports Physician.” Learn more at www.FootLevelers.com.
1. Dahlhamer, James, et al. “Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016/’ Morbidity and Mortality Weekly Report, vol. 67, no. 36, 2018, pp. 1001-1006.
2. Latremoliere, Alban, and Clifford J. Woolf. “Central sensitization: a generator of pain hypersensitivity by central neural plasticity.” The Journal of Pain, vol. 10, no. 9, 2009, pp. 895-926.
3. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 [published correction appears in Lancet. 2017 Oct 28; 390(10106):e38]. Lancet 2017;390:1211-59.
4. Paige, Neil M., et al. “Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain.” BMJ, vol. 364, 2019, 1689.
5. Rubinstein, Sidney M., et al. “Spinal manipulative therapy for chronic low-back pain.” Cochrane Database of Systematic Reviews, no. 9, 2020, CD008112.
6. Bialosky JE, George SZ, Hom ME, Price DD, Staud R, Robinson ME. Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain (NCT01168999). J Pain. 2014 Feb; 15(2): 136-48. doi: 10.1016/jjpain.2013.10.005. Epub 2013 Oct27. PMID: 24361109; PMCID: PMC3946602.
7. Kim D, Cho M, Park Y, Yang Y. Effect of an exercise program forposture correction on musculoskeletal pain. J Phys Ther Sci. 2015 Jun;27(6): 1791-4. doi: 10.1589/jpts.27.1791. Epub 2015 Jun 30. PMID: 26180322; PMCID: PMC4499985.
8. Akuthota, Venu, and Scott F. Nadler. “Core strengthening.” Archives of Physical Medicine and Rehabilitation, vol. 85, no. 3, 2004, pp. S86-S92.
9. Qaseem, Amir, et al. “Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians.” Annals of Internal Medicine, vol. 166, no. 7, 2017, pp. 514-530."
10. Fernandez MI, Watson PJ, Rowbotham D J. Effect of pulsed magnetic field therapy on pain reported by human volunteers in a laboratory model of acute pain. Br JAnaesth. 2007 Aug;99(2):266-9. doi: 10.1093/bja/aeml29. Epub 2007 May 22. PMID: 17519258
11. Hamblin, Michael R. “Mechanisms and applications of the anti-inflammatoryeffects of photobiomodulation.” AIMS Biophysics, vol. 4, no. 3, 2017, pp.337-361.
 View Full Issue
View Full Issue