Dr. Welby Goes Breaking Bad
FEATURE
JC Smith
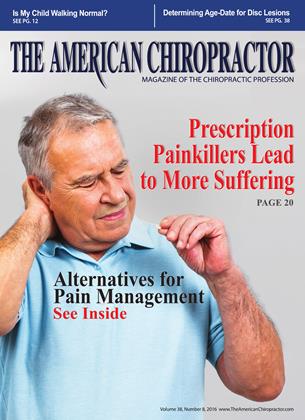
Once again, the unrelenting campaign by Big Pharma to drug Americans at any cost and any consequence for big profits has come to light as more dangerous and pervasive than anyone realizes.
Time magazine finally revealed in its June 4, 2015, cover story by Massimo Calabresi, “The Price We Pay for Relief: Whv America Can’t Kick Its Painkiller Problem.” the massive overdosing of Americans with opioid painkillers.
It is interesting to note the author admits “America can’t kick its painkiller problem” rather than offering solutions for “how to kick this painkiller problem,” such has chiropractic care as the logical nondrug solution for any spine-related disorder, which is the largest disabling condition in the nation, military, and the world. Indeed, back pain is a huge problem that has gone relatively unnoticed by the media.
For example, the Global Burden of Disease Study involves data from 188 countries and looks at 301 illnesses and injuries for 21 regions covering the entire globe. In 1990, the leading causes of ill health worldwide included low back pain, depression, iron-deficiency anemia, neck pain, and age-related hearing loss.
Again in 2013, two conditions—musculoskeletal problems (mainly conditions such as low back pain, neck pain and arthritis) and mental health/substance abuse disorders (mainly depression, anxiety, and drug and alcohol abuse) accounted for nearly half of all loss of healthy years of life, the report said.1
“Large, preventable causes of health loss, particularly serious musculoskeletal disorders (MSDs) and mental and behavioral disorders, have not received the attention that they deserve,” noted study author Theo Vos, professor of global health at the Institute of Health Metrics and Evaluation at the University of Washington.2
This will remain a huge problem to kick considering two of the biggest economic forces in America are involved—Big Pharma and Big Medicine. Both have a financial incentive to continue drugging people and neither has any interest to promote a nondrug solution for anything. Addictions, deaths, bribes, and lawsuits are just the cost of doing business for the medical industrial complex to keep its grip on Americans.
This issue is plainly another medical boondoggle, which, for your information, is defined by Merriam-Webster as “a wasteful or impractical project or activity often involving graft.” As I pointed out with numerous examples in my past
article. “Medical Payola.” this boondoggle within medicine is not a new story, just another page in the same script that has been playing for decades across America starring the standard actors touting “wonder drugs” and “heroic surgeries” as the only solutions to health problems.
Patients’ Purple Haze
Many new patients with MSDs who come to thousands of chiropractic practices throughout the country invariably have tried the sequence of chemical painkillers already—OTC medications, steroid injections, and then prescription opioid painkillers. Most people seem to be in a purple haze on the issue of opioid painkillers—confused, bewildered, or just stoned.
To my surprise, few realize these painkillers have a similar chemical structure to heroin. When I inform them of this fact, which explains why it is called the “hillbilly heroin” epidemic, their jaws hit the floor because their MDs and pharmacists failed to inform them. Most mistakenly think it’s just another stronger aspirin-type painkiller.
Apparently handing out heroin is the equivalent of handing out Halloween candy to patients.
Even more shocking, I have discovered VA patients are required to initially take opioids and have steroid injections before they are referred to my office for a nondrug solution.
As one vet told me, if these veterans do not have opiates in their blood when tested periodically, they are reprimanded for malingering! How convoluted has the VA become?
For your information, common opioids by brand names include hydrocodone (Vicodin), hydromorphone (Dilaudid), meperidine (Demerol), methadone (Dolophine), morphine (Roxanol), oxycodone (OxyContin, Percocet), and perhaps the worst, oxymorphone (Opana), a new form that could be driving abusers to inject the drug intravenously instead of snorting it.
Don’t count on the federal government to police these heroin products. For its part, the FDA continues to behave as if the answer to the opioid epidemic is stronger opioids.
In 2013, the FDA approved an extended-release drug called Zohydro, which is 25% more powerful than Opana and has no abuse-deterrent properties. In fact, the FDA overruled its own safety advisory board, which had voted 11 to 2 against approval because of addiction concerns. A year later, in
“To my surprise, few realize these painkillers have a similar chemical structure to heroin. J J
November 2014, the FDA approved Hysingla, which has abuse-deterrent properties but is twice as powerful as Opana.3
Nor does the AMA or Big Pharma want a nondrug solution for back pain mentioned on television, and the drug lords certainly have the money to get what they want with the media. According to a study in the New England Journal of Medicine, “Total real spending on promotion grew from $11.4 billion to $29.9 billion from 1996 to 2005, at an average annual rate of 10.6%...Real spending on direct-to-consumer advertising increased by 330% from 1996 to 2005.”4
FDA = Fun Drugs for All
Indeed, Americans have been led down the primrose path to the worst health statistics among the advanced nations of the world according to the Commonwealth Fund Scorecard.5 However, they will never know because the commercial media continues to reinforce the myth that “America has the best healthcare system in the world,” as Big Pharma sells them the underlying mantra, “a pill for every ill.”
In the Time article, writer Calabresi gave what should be the lead-in to our profession’s pitch:
“This is not a story about dark alleys and drug dealers. It starts in doctors’ offices with everyday people seeking relief from pain and suffering. Around the nation, doctors so frequently prescribe the drugs known as opioids for chronic pain from conditions like arthritis, migraines, and lower-back injuries that there are enough pills prescribed every year to keep every American adult medicated around the clock for a month. The longer patients stay on the drugs, which are chemically related to heroin and trigger a similar biological response, including euphoria, the higher the chances users will become addicted.”6
As he writes, “It starts in doctors’ offices with everyday people seeking relief from pain and suffering.” Plus, the so-called “relief’ offered in medical offices is an illusion since these drugs do not correct the underlying source of pain and are temporary at best with dangerous long-term side effects, such as addiction, disability, and death
considering 46 people die daily from prescription painkillers in the US according to the CDC.7
We should emphatically add that patients are in the wrong type of doctor’s office when they should be in a chiropractor’s office instead for the majority of MSDs. Indeed, the public and press need to learn that chiropractors have their backs instead of medical primary care physicians (PCPs) who have been shown to be “inept” in academic training on musculoskeletal disorders,8 are more likely to ignore recent guidelines,9 and are more likely to suggest spine surgery than surgeons themselves.10
Rather than being seen as an authority on chronic pain, more evidence emerges revealing that many MDs are scamming the public’s need for relief with drugs that are short term and placebo at best, and at their worst, dangerous, addictive, and often deadly. Instead of leading them to narcotic medications, if the stereotypical Marcus Welby, MD, had any semblance of ethics to “first do no harm,” he or she would refer patients with acute and/or chronic musculoskeletal pain to chiropractors as almost every guideline now recommends.
However, just as we witnessed with Dr. Sanjay Gupta’s program on CNN, Deadly Dose, this recent Time magazine article made no reference to chiropractic care. Once again, we are off the media’s radar as the logical solution to the “hillbilly heroin” epidemic, as people on Main Street refer to this opioid pandemic.
The Time writer also offered a poignant summary of this bleak situation:
“It took a tragic combination of good intentions, criminal deception, and feckless oversight to turn America’s desire to relieve its pain into such widespread suffering. Most everyone has played a role. Weak research opened the door to overuse of opioids. The Food and Drug
Administration (FDA) approved ever more powerful drugs for long-term use based only on evidence of their short-term safety and efficacy. Two pharmaceutical companies pleaded guilty to criminal charges that they misleadingly marketed the drugs as safe. Too many doctors embraced the easy solution of treating pain by writing a prescription.”11
An easier and more effective solution would be to refer these cases to chiropractors, but the medical spine complex has no intention of losing its huge market share in the spine business, even if patients would benefit. Indeed, the medical war against chiropractors continues to this day and patients are merely the collateral damage of this onslaught of drug, shots, and surgery.
Moreover, the medical co-conspirators have not stepped up to admit their complicity in this matter. “No one anticipated the clinical community would take to this and start giving it out like water,” said Janet Woodcock, head of the FDA’s Center for Drug Evaluation and Research.
Not just any water, but very expensive water since the total annual sales for opioids in the US has grown over the course of the past 20 years to more than $8 billion, according to the Time article, not counting the illicit money made by pushers on the street. This largesse does not include office visit fees enjoyed by pill-mill doctors, a cash cow neither Big Pharma nor the AMA wants to see dry up.
In Your Back Yard
This opioid pandemic is happening everywhere in the US, not only in Kentucky, Indiana, West Virginia, and Florida, which have gotten the most attention in the media lately.
For example, recently in the Macon area, George M. Bird, MD, and his nurse were arrested in a pill-mill operation where authorities found almost $1 million in cash stashed in boxes and a duffel bag. In all, some $3 million in assets were seized, including two offices, a house, and four automobiles.12
In a similar bust in 2008 in middle Georgia, Dr. Spurgeon Green received a 30-year federal prison sentence for illegally prescribing “narcotic cocktails”—Oxycodone and other schedule-II drugs to any “patient” who could pay cash. Acting US Attorney G. F. “Pete” Peterman stated that the volume of narcotics dispensed by Green was “10 times higher than the national doctor average.”13
According to the summary by the United States Court of Appeals, Eleventh Circuit, from 1992 to 2003, Green operated a medical clinic in Perry, Georgia. Houston County police became suspicious that Green’s medical clinic was not an ordinary doctor’s office after they received complaints about long lines of people waiting outside the clinic. Police conducted surveillance of the clinic and observed that the parking lot outside the clinic was often full of patients, many from out of state, waiting to see Green. Search of his home
later found about $800,000 in cash. When asked why he had so much money, he told the local press he didn’t trust banks.
From the case summary decided February 21, 2013, the depth of Dr. Green’s pill mill is more shocking than even Time magazine portrayed. The prosecution presented evidence at trial that Green’s medical practice and his clinic were unusual in many respects. Green saw as many as 100 patients each day. He required that his patients pay in cash or by credit card before they met with him, and he did not accept private insurance. Inside the clinic, patients were sometimes rude and hysterical. Some patients could be heard retching in the bathroom, while other patients offered the receptionists bribes to see the doctor as soon as possible. Outside the clinic, patients sometimes camped overnight, sleeping in cars and urinating in public.
Many of Green’s former patients were addicted to prescription drugs or sold their prescription drugs to addicts. These patients went to Green’s clinic because they knew he would give them the prescription drugs they wanted. One former patient testified that it was “common knowledge that you could go to [Green] and basically write a grocery list [of] what you needed, and, you know, he would fill it.” Another former patient addicted to prescription drugs testified that her “honest opinion was it was a dope house,” and she testified that “people were getting sick in the bathroom. There were drug deals going on in the parking lot.”
Dr. Barry Straus, an expert in pain management and the prescription of controlled substances who was a practicing physi-
■ "However, if pain management doctors were to follow the latest guidelines for acute low back pain in adults they should refer their spine-related pain patients to chiropractors for conservative, nondrug treatments initially.??
cian in Georgia, testified that there aie standards in the practice of pain management, and he explained how doctors must treat their patients to comply with those standards.
Dr. Straus testified that doctors should consider ways to treat pain other than through narcotics treatment, and that it is customarily inappropriate for a physician to treat a patient by immediately prescribing him a controlled substance. He said if the doctor decides to prescribe a controlled substance, he should move “up the ladder” and begin his treatment by distributing less powerful and less addictive drugs.14
The jury convicted Green on 46 counts of violating or conspiring to violate the Controlled Substances Act, including one count of unlawfully dispensing or distributing controlled substances and causing death or serious bodily injury. His physician assistant and pharmacist were also found guilty. Following his sentencing of 30 years in prison, Dr. Green told news reporters, “Now I know how Jesus felt.”15
Dr. Green’s comment illustrates the delusion most pain management practitioners have, even those not as egregious who have not yet been prosecuted. They know narcotics and ESIs only mask pain temporarily, but they have no qualms about rendering ineffective services as long as they are making money. And with a public clamoring for quick fixes, they are happy to oblige them.
Dr. Welby Goes Bad
However, if pain management doctors were to follow the
latest guidelines for acute low back pain in adults they should refer their spine-related pain patients to chiropractors for conservative, nondrug treatments initially. [16] The negligible likelihood of this referral is a remnant of the AMA’s boycott of chiropractic that has contributed to this massive opioid abuse we now witness as well as the overuse of epidural steroid injections, MRIs, and, of course, spine fusions.
Perhaps the bigger question is why does insurance pay for these ineffective treatments while limiting chiropractic care? This “perverse” motivation is the driving force behind this medical scam; indeed, if insurance did not pay, most patients would never have started down that dangerous path to opioid addiction.
Do we wonder anymore why back pain is the number one disabling condition in the nation, military, and in the world when the medical profession so terribly mismanages these cases with opioids, ESIs, and disc fusions?
People have no idea the extensive and dangerous nature of this epidemic:
“Of the 9.4 million Americans who take opioids for longterm pain, 2.1 million are estimated by the National Institutes of Health to be hooked and are in danger of turning to the black market. Now 4 of 5 heroin addicts say they came to the drug from prescription painkillers. An average of 46 Ameri-
cans die every day from prescription-opioid overdoses, and heroin deaths have more than doubled to 8,000 a year, since 2010. For middle-aged Americans, who are most at risk, a prescription-opioid overdose is a more likely cause of death than an auto accident or a violent crime.”17
Calabresi made it clear in Time that the FDA, Big Pharma, and the AMA have no interest to stop this tsunami of opiates; even if they did (okay, stop laughing), there is no way to end this legal inebriation of Americans who would undergo withdrawals and take to the streets for heroin. He mentions that something needs to done, but he doubts medical associations will take the responsible role:
“All now agree that the opioid epidemic is a terrible problem, but few ai e taking responsibility. It has fallen to local law enforcement and health professionals to clean up the mess as addiction and abuse ravage their communities. It’s not easy. The same medical associations that once pressured doctors to hand out opioids liberally now issue conflicting advice over how to combat the problem they helped create. Government scientists admit they have no idea when and whether it’s safe to use opioids to treat long-term pain.”18
Whether it’s medicinal pot, medicinal heroin, or their recreational equivalents on the street, people want their high regardless if pushed or prescribed. And using “pain management” as an excuse to get their narcotics is easier than walking the
streets since all you have to do is walk into a doctor’s office. Plus, it’s legal and insurance pays for it!
Thomas Frieden, MD, the director of the CDC, commented in 2011 about “the burden of dangerous drugs” in medicine. Considering one in 20 American adults is now addicted to prescription narcotics, he said physicians have supplanted drug pushers on the street corners as the most important suppliers of illicit narcotics.19
Indeed, Dr. Marcus Welby has joined the cast of Breaking Bad.
Speak Up Chiropractors
This huge pandemic of pain and the downside of prescription painkillers is a golden opportunity for the chiropractic profession to speak out in the “earned media” rather than paying for advertisements. It would open the door to an intelligent, in-depth conversation on television or radio news programs of the overall status of back pain care in American healthcare.
A talking point for our chiropractic lobbyists and PR campaigns needs to be based on an anti-opioid theme. This should also be a serendipitous public relations opportunity for the chiropractic profession to showcase itself as the nondrug solution to the pandemic of painkillers, shots, and surgery. Our national associations in conjunction with the F4CP need
to step up to the plate with spokespeople to comment on the value chiropractic presents to this national opioid boondoggle.
This anti-opiate pitch would logically lead to the anti-ESI, anti-MRI, and most of all, anti-spine fusion topics. Indeed, Americans have yet to learn of the debunking of disc fusions despite the research showing “bad discs” appear in pain-free people as the recent Mayo Clinic review agreed.20 Oddly, this Mayo review got no traction in the mainstream media.
In fact, researchers now agree that most back pain is mechanical in nature (pathophysiologic) and not due to “bad discs” (pathoanatomic). In other words, how the spine actually functions is much more important than how it looks on an image, an important message the public has yet to understand.
Despite research back in 1990 confirming this, the public remains victimized by unscrupulous surgeons selling “red herrings,” as Dr. Donald Murphy21 suggests, that are used as a sales pitch to convince naïve patients these “incidentalomas” are significant when, in fact, they may actually be “coincidentalomas” with undiagnosed joint dysfunction at the same level.
If and when our profession gets this revolutionary science to the public, they may finally understand that chiropractors were on the right track all along by offering a nondrug solution to spine-related musculoskeletal disorders, a huge market with millions of potential patients and billions of dollars at stake.
If the public knew the truth as it already is known by many medical journalists, back pain is an epidemic that has been mismanaged by the medical profession to the point where Mark Schoene, associate editor of The Backletter, an international spine research journal, declared, “Spinal medicine in the US is a poster child for inefficient care.”22
Let’s use this Time magazine cover story as a breakthrough event to tell the chiropractic story. The F4CP now has an opportunity to use this information in their media campaign to educate the public. Hopefully, our new campaign will gain some traction in the earned media, but it won’t without a big push back by the chiropractic profession.
References:
1. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013, The Lancet, published Online: 07 June 2015.
2. The Lancet, news release, June 8, 2015
3. Massimo Calabresi, The Price We Pay for Relief: Wiry America Can \ Kick Its Painkiller Problem, Time, June 4, 2015
4. Julie M. Donohue, Ph.D., Marisa Cevasco, B.A., and Meredith B. Rosenthal, Ph.D., A Decade ofDirect-to-Consumer Advertising of Prescription Drugs, N Engl JMed2007; 357:673-681August 16, 2007DOL 10.1056/NEJMsa070502
5. http://www.commonwealthfund.org/publications/fund-reports/2014/jun/ mirror-mirror
6. Massimo Calabresi, The Price We Pay for Relief: Wiry America Can \ Kick Its Painkiller Problem, Time, June 4, 2015
7. CDC Vital Signs, http://www.cdc.gov/vitalsigns/pdf/2014-07-vitalsigns.pdf
8. EA Joy, S Van Hala, “Musculoskeletal Curricula in Medical Education— Filling In the Missing Pieces, The Physician And Sports Medicine, ” 32/11 (November 2004).
9. PB Bishop et al., “TheC.H.I.R.O. (Chiropractic Hospital-Based Interventions Research Outcomes) part I: A Randomized Controlled Trial on the Effectiveness of Clinical Practice Guidelines in the Medical and Chiropractic Management of Patients with Acute Mechanical Low Back Pain, ”presented at the annual meeting of the International Society for the Study of the Lumbar Spine Hong Kong, 2007; presented at the annual meeting of the North American Spine Society, Austin, Texas, 2007; Spine, in press.
10. SS Bederman, NN Mahomed, HJ Kreder; et al. “In the Eye of the Beholder: Preferences of Patients, Family Physicians, and Surgeons for Lumbar Spinal Surgery, ” Spine 135/1 (2010):108-115
11. Massimo Calabresi, The Price We Pay for Relief: Why America Can’t Kick Its Painkiller Problem, Time, June 4, 2015
12. “Nearly $ 1M cash seized in alleged midstate ‘pillmill’bust, ” MaconTelegraph staff report, June 6, 2105.
13. See more at: http://caselaw.findlaw.eom/us-llth-circuit/1624098.html#sthash. iThsqour.dpuf
14. [14] http.V/caselawfindlaw.com/us-11 th-circuit/1624098.html#sthash.iThsqour.dpuf
15. bainbridgega.com/news/publish/080509drgreen.shtml
16. Bigos S. étal. USDept. ofHealth and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, December 1994.
17. Massimo Calabresi, The Price We Pay for Relief: Wiry America Can \ Kick Its Painkiller Problem, Time, June 4, 2015
18. Massimo Calabresi, The Price We Pay for Relief: Why America Can’t Kick Its Painkiller Problem, Time, June 4, 2015
19. Centers for Disease Control and Prevention Press Release, CDC Dial Signs: Overdose of Prescription Opioid Pain Relievers—United States, 1999-2008; 2011 :www. cdc.gov/media/releases/2011/tll 01 _presecription_pain_relievers. htrnl.
20. Brinjikji W, et al., Systematic literature review of imaging features of spinal degeneration in asymptomatic populations, American Journal of Neuroradiology, 2014, prepub ahead of print;www.ajnr.org/content/early/2014/ll/27/ ajnr.A4173.long.
21. DRMurphy, Clinical Reasoning in Spine Pain volume 1, Primary Management of Low Back Disorders Using the CRLSP Protocols © Donald Murphy 2013, p. viii
22. The Backletter editorial vol. 27, No. 11, November 2012.
JC Smith, MA, DC, is a 35-year practicing chiropractor, author of The Medical War Against Chiropraetors, and he maintains a website, Chiropractors for Fair Journalism.
 View Full Issue
View Full Issue