Chiropractic Spinal Adjustments and the Effects on the Neuroendocrine System and the Central Nervous System Connection
FEATURE
A literature review and report
By: Mark Studin, DC, FASBE(C), DAAPM, DAAMLP William Owens, DC, DAAMLP, CPC
Chiropractors have long held the notion that “people get well and stay well at a higher level because of chiropractic care.” This has been the mantra of the primary author for more than 30 years and has been based upon the observation of thousands of patients reporting the effects of chiropractic care, an integral part of the definition of “best medical practice.” Although this is a chiropractic forum, we must never forget that we are part of the medical genre in society and fall under the same standards as all other forms of health care. The public perceives the term “medical” to be synonymous with “health care,” and by understanding that, it means we are better able to communicate with our patients and other providers in our area.
“A best practice is a method or technique that has consistently shown results superior to those achieved with other means, and that is used as a benchmark. In addition, a ‘best’ practice can evolve to become better as improvements are discovered. Best practice is considered by some as a business buzzword, used to describe the process of developing and following a standard way of doing things that multiple organizations can use” (Best Practice, 2015, http://en.wikipedia. org/wiki/Best practice).
Best practices in health care include the examination and treatment procedures that are taught in schools, internships, and residencies, and are considered the standard protocols and the foundation by which healthcare providers operate. These practices are based on clinical experience and rely heavily on time-tested approaches. This is one of the major reasons why experience matters. Surprisingly, most of the best medical practice care paths are not published in the peer-reviewed indexed literature. This is due to many factors, although the most obvious one is the global application of financial resources to “new” discoveries. The clinical arena is generally adequate to monitor and adjust these “new findings” within healthcare practices in a timely manner to keep up with the literature that follows. In recent times, although the concept has been talked about for decades, there has been an additional parameter put into play—a strong reliance on published studies (also known as evidence) as the main driver of whether
a procedure is utilized or not, particularly by payers. This is extremely problematic to healthcare outcomes because it is only one portion of the evidence-based paradigm, leaving clinical experience and patient response to care out of the picture. Many leaders suggest it is a focus on cutting costs as opposed to providing the best health care possible.
The primary author states, “I must admit that through the years, although I had practiced in a purely best-practice paradigm, I was in a dogmatic mindset where nothing could shake my belief, yet my observations validated my beliefs on a daily basis with results that couldn’t be explained in the literature. These observations were that many patients got over their illnesses with direct, immediate, and predictable relationships to the chiropractic adjustments they received, yet the only
evidence was these observations, and there was nothing to support them in the research. Today, that is changing rapidly, and now we have evidence of measurable changes secondary to chiropractic adjustments with measurable central nervous system and physiological changes.”
In order to fully understand the effects of the spinal adjustment on the function and potential disease processes, we must first understand there are three primary pathways by which the chiropractic adjustment affects the human body. These aie through biomechanics (local joint fixation and motion), pain management (organized and monitored through sensory input into the dorsal horn of the spinal cord to higher centers in the brain), and the autonomic systems (sympathetic and parasympathetic influences such as blood pressure changes through the endocrine system). We have discussed the first two pathways in detail in other recent articles and lectures, but in this paper, we need to define and understand both the endocrine and neuroendocrine systems because they are the pathway through which the mechanisms function and potentially break down. Then we must explore the evidence of how a spinal adjustment affects the hormonal systems and realize that what chiropractors do goes well beyond the positive effects of treating mechanical spine pain.
According to the Canadian Cancer Society in discussing the anatomy and physiology of the neuroendocrine and endocrine systems:
The neuroendocrine system is made up of a network of cells that aie distributed throughout the body. The word neuroendocrine refers to two qualities of these cells: they have a similar structure to nerve cells (neurons) and produce hormones like endocrine cells. Neuroendocrine cells release hormones into the bloodstream in response to chemical signals from other cells or messages from the nervous system [a chemical communication process]. These hormones work like neurotransmitters. Neurotransmitters ai e chemicals released by a nerve cell to transmit signals or impulses from one nerve cell to another nerve cell or other specialized cells.
[The neuroendocrine system is formed by two distinct portions and it can be a little confusing. The divisions aie the diffuse neuroendocrine system and the endocrine system.]
The diffuse neuroendocrine system is made up of neuroendocrine cells scattered throughout the body.
[Here are a few examples to help you understand the process and system.]
• Neuroendocrine cells in the digestive system regulate intestinal movements and the release of digestive enzymes.
• Neuroendocrine cells in the respiratory system aie believed to play a role in the developmental stages of the respiratory organs. They also regulate respiratory function.
• There are small neuroendocrine organs, known as paraganglia, along the spinal column. They include the adrenal medulla inside the adrenal gland and paraganglia outside
the adrenal gland. They produce the hormones epinephrine and norepinephrine. These hormones control blood pressure and heart rate.
• Neuroendocrine cells are also found in non-neuroendocrine glands and are scattered in the skin, thymus, prostate and other tissues.
• The endocrine system is formed by the endocrine glands, which are ductless glands that secrete hormones directly into the blood or lymph fluid. The actions of these hormones vary according to the gland and specific type of hormone produced.
• The endocrine system is made up of pituitary, pineal, thyroid, parathyroid and adrenal glands, pancreatic islet cells (also known as islets of Langerhans) and the ovaries or testicles.
• The pituitary, pineal and parathyroid glands are neuroendocrine glands.
• The thyroid gland is not a neuroendocrine gland, but it contains scattered neuroendocrine cells known as C cells.
• The adrenal glands ai e made up of a non-neuroendocrine area called the cortex, and a central neuroendocrine gland called the medulla.
• The pancreas is an exocrine gland, but contains scattered groups of neuroendocrine cells called pancreatic islets.
• The ovaries and testicles are not neuroendocrine glands, but contain scattered neuroendocrine cells.
travel throughout the body to reach their target cells. Each type of hormone binds to a specific receptor on the target cell. The target cell responds to this hormone by changing specific cellular functions, such as metabolism, growth and reproduction. Complex feedback mechanisms involving the nervous system, endocrine system and diffuse neuroendocrine system control the levels of hormones in the body, (http://www.cancer.ca/en/ cancer-information/cancer-type/neuroendocrine/anatomy-andphysiology/?region=on)
■ "In order to fully understand the effects of the spinal adjustment on the function and potential disease processes, we must first understand there are three primary pathways by which the chiropractic adjustment affects the human body. J J
Neuroendocrine cells are highly specialized nerve-like cells that release hormones in response to a neurological or chemical signal. The hormones released by the cells enter the blood and
It has been well established, as reported by Studin, Owens, and Zolli (2015), that the chiropractic spinal adjustment has a direct and immediate effect on the central nervous system, outlined as part of the “pain management” pathway of the
chiropractic spinal adjustment response. Research has shown that the chiropractic spinal adjustment affects the modulation of ascending and descending communication in the central nervous system within the dorsal hom. The adjustment then affects the thalamus and other areas of the brain, and it has a direct effect on gating pain in both directly treated and disparate regions because of the central nervous system connections. There are ancillary effects within primitive centers of the brain that control anxiety, depression, and chronic responses to pain.
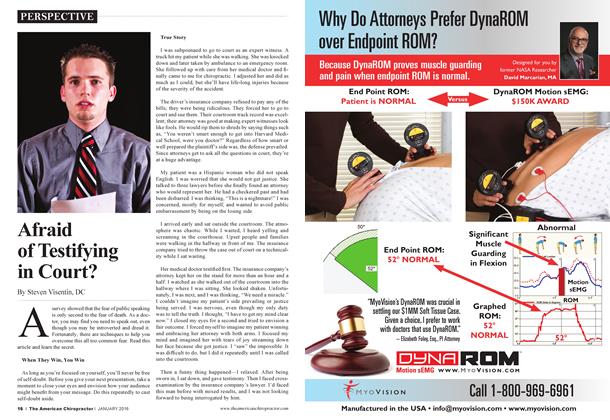
Kovanur Sampath, Mani, Cotter, andTumilty (2015) reported that the effects of spinal manipulation (chiropractic spinal adjustments) on various functions of the autonomic nervous system have been well identified in manual therapy literature. They reported, “The common physiological mechanism proposed for these ANS changes involves possible influence on segmental and extrasegmental reflexes with a prominent role given to the peripheral sympathetic nervous system” (p. 2). They reported the following outcomes as measuring tools of the peripheral sympathetic nervous system:
1. Skin blood flow
a. Skin temperature
b. Skin conductivity
c. Laser Doppler flowmetry
2. Plethysmography (checks for lung tidal air and possible blood clots)
3. Blood pressure changes
4. Pupillary reflexes
5. Heart rate variability
Based upon the studies using these measuring tools, Kovanur Sampath et al. (2015) concluded that “cervical manipulation elicits a parasympathetic response and a thoracic/lumbar SM [spinal manipulation] elicits a sympathetic response” (Kovanur Sampath et ah, 2015, p. 2). In summary, it is evident that spinal manipulation has an effect on the autonomic nervous system, though the direction of effect may vary. While we have spent years observing and studying the effects of the chiropractic spinal adjustment, there has never been an identified direct connection to the higher cortical areas until recently. Published research specifically involving the cerebellar vermis (the area connecting the two hemispheres of the brain) that is directly involved in mental stress, proprioception, and the autonomic nervous system aie being published at an unprecedented rate.
Kovanur Sampath et al. (2015) continued, “A chiropractic study investigated the status of regional brain activity immediately after a cervical SM [spinal manipulation]. In a cross-over trial, 12 men with neck pain and shoulder stiffness were assigned to the treatment and the resting conditions. Positron Emission Tomography (PET) was used in the study to examine the regional cerebral metabolism. The researchers noted significant changes in the cerebellar vermis, which was deactivated in the treatment condition compared to the resting condition... Removal of the cerebellum impairs performance of autonomic functions including salivary, cardiac and respiratory conditioning. Further, other areas of the brain such as the anterior cingulate cortex, inferior prefrontal cortex, and middle temporal gyrus were also activated in the treatment condition compared to the resting condition. All these areas of the brain
are involved in the generation of autonomic responses. Hence the authors argued that activation of the anterior cingulate cortex combined with deactivation of the cerebellar vermis resulted in reduced sympathetic tone and pain levels” (Kovanur Sampath et al.,
2015, p. 2-4). This is the start of understanding how regional brain activity creates profound changes in the human central nervous system, and that, in fact, it can be influenced directly by the chiropractic adjustment.
Kovanur Sampath et al. (2015) continued:
Recently, another imaging study investigated if supraspinal activation in response to noxious stimuli varied preand postthrust manipulation to the thoracic spine. Using functional magnetic resonance imaging (fMRI), the researchers imaged various areas of the brain during a thoracic spinal manipulation. The results of the study revealed significant reduction of activation in the insular cortex and anterior cingulate cortex. The reduction in activation of the insular cortex was correlated with a significant reduction in subjects’ perception of pain. The insular cortex and the anterior cingulate cortex are both engaged in pain processing and both participate in high-level control of autonomic function. Although these two areas are intercon-
■ "Through its projections to many components of the central autonomic network, stimulation of insular cortex elicits changes in all autonomic functions. J J
nected, they operate independently and analyze different components of pain sensation.
Insular cortex, as paid of the limbic system is involved in detecting saliency of sensory information, memory and pain perception, and in selective transmission of this information to other areas within the pain matrix. Through its projections to many components of the central autonomic network, stimulation of insular cortex elicits changes in all autonomic functions. The primary function of anterior cingulate cortex is to predict and avoid noxious stimuli... depending on which column (lateral or medial) is activated, sympathoexcitation or sympathoinhibition may be produced. Taken together, the evidence clearly points out that spinal manipulation will have an effect (excitatory or inhibitory) on the ANS [autonomic nervous system], (p. 3)
As a result of the previous scenario, Kovanur Sampath et al. (2015) have taken the next step and reported, “We proposed that a SM [spinal manipulation, chiropractic spinal adjustment] of the thoracic spine in humans will be associated with a neuro-endocrinal response. Substantial evidence has demonstrated the neurophysiological effects of SM, with a prominent role given to the SNS [sympathetic nervous system]. Recent systematic reviews further confirm the short-term sympathoexcitatory effects associated with SM. These SNS changes following SM may also be associated with changes in supraspinal mechanisms that control pain. Supraspinal structures such as the anterior cingular cortex, amygdala, PAG [periaqueductal gray matter], RVM [rostral ventrolateral medulla] and cerebellar vermis have been implicated in manipulation induced analgesia and concurrent autonomic effects” (Kovanur Sampath et ah, 2015, p. 4).
Unlike pain modulation where the region treated does not always show a direct cause and effect response, autonomic responses suggest that, depending upon the region adjusted and stimulated, it will determine the outcome and changes. The literature, according to Kovanur Sampath et al. (2015), has concluded that there is a direct relationship between the autonomic system and the hypothalamus-pituitary-adrenal gland in chronic pain syndromes, including autoimmune diseases such as fibromyalgia, diabetes, gastrointestinal disorders, cardiovascu-
lar problems, and asthma. Currently, research is finally linking the neuronal mechanisms involved in pain modulation to the chiropractic adjustment with the newest research connecting the neuroendocrine pathways to chiropractic as outlined previously. The next step is to measure the endocrine output after chiropractic care in the resultant effector organs in both healthy individuals and those in a diseased state. The key is utilizing the chiropractic spinal adjustment in balancing the autonomic nervous system and, in turn, helping to rectify the hypothalamus-pituitary-adrenal gland imbalance as a viable treatment modality.
In conclusion, neuroendocrine pathway research has the ability to bring chiropractic full circle to proving objectively and scientifically what we have observed for 120 years. These aie exciting times for our profession and our patients.
References:
Best Practice. (2015). Wikipedia. Retrieved from http:// en.wikipedia.org/wiki/BestjDractice
Anatomy and Physiology of the Neuroendocrine System, (n.d.). Canadian Cancer Society. Retrieved from http://www.cancer.ca/ en/cancer-information/cancer-type/neuroendocrine/anatomy-andphy si ol ogy/?regi on=on
Studin, M., Owens, W., Zolli, F. (2015). Chiropractic, chronic back pain and brain shrinkage: Abetter understanding of Alzheimer’s, dementia, schizophrenia, depression and cognitive disorders and chiropractic’s role—A literature review of the mechanisms. The American Chiropractor, 37(10), 36-38, 40-42, 44-45.
Kovanur Sampath, K., Mani, R., Cotter, J. D, & Tumilty, S. (2015). Measurable changes in the neuro-endocrine mechanism following spinal manipulation]. Medical Hypothesis, [epub ahead of print, October 7, 2015], Retrieved from http://www.medical-hypotheses. com/article/S0306-9877%2815%2900374-6/abstract.
Dr. Mark Studin is an adjunct associate professor of chiropractic at the University Of Bridgeport College Of Chiropractic, an adjunct professor of clinical sciences at Texas Chiropractic College, and a clinical presenter for the State of New York at Buffalo, School of Medicine and Biomedical Sciences for postdoctoral education, teaching MRI spine interpretation and triaging trauma cases. He is also the president of the Academy of Chiropractic teaching doctors of chiropractic how to interface with the legal community (www.DoctorsPIProgram. com), teaches MRI interpretation and triaging trauma cases to doctors of all disciplines nationally, and studies trends in health care on a national scale (www. TeachDoctors.com). He can be reached at DrMark a A cademyofChiropractic.com or at 631-786-4253.
Dr Bill Owens is presently in private practice in Buffalo and Rochester, New York, and generates the majority of his new patient referrals directly from the primary care medical comm unity. He is an associate adjunct professor at the State University of New York at Buffalo School of Medicine and Biomedical Sciences as well as the University of Bridgeport, College of Chiropractic, and an adjunct professor ofclinical sciences at Texas Chiropractic College. He also works directly with doctors of chiropractic to help them build relationships with medical providers in their communities. He can be reached at dr. owensra academyc fchiropractic. com, www. mdreferralprogram. com, or 716-228-3847.
 View Full Issue
View Full Issue