Getting to the Bottom of Pelvic Problems
By Dr. George Roth, DC, ND, CMRP
The Importance of the Pelvis
As healthcare providers, we may have studied the anatomy of the pelvis by reading books, observing skeletal models, performing dissections, or examining patients. However, we most likely overlooked the effects many common injuries have on this part of the body, leading to pelvic dysfunction.
Pelvic dysfunction can include biomechanical issues affecting the lumbar spine, sacroiliac joints, hip joints, and lower extremities. Common conditions, such as lumbar disc degeneration resulting in low back pain, hip degeneration, and arthritis of the knees, provide an endless stream of patients who are prescribed medication and inevitably wind up going under the surgeon’s scalpel.
My clinical experience also indicates that pelvic dysfunction contributes to various visceral conditions. Urinary incontinence alone affects approximately 5% of the world’s population, while dysmenorrhea affects approximately 50% of women of reproductive age,2 and one in five men will experience erectile dysfunction at some point in their lives.1-3
So why is pelvic dysfunction prevalent, and how can we address it?
To understand why this issue is becoming more of a problem with each passing year, we need to understand how the pelvis and many other parts of the body might be affected by some common injuries.
The Physics of Impact Injury
As an assistant instructor in human dissection, I noticed almost 50 years ago that bone size differed on one side of the body compared to the same structure on the opposite side. These observations were later verified as the result of impact injury to bone.4 This is crucial to understanding how injury affects biomechanics and physiology.
When considering how these injuries occur, we should recall that homo sapiens are unique in the animal kingdom because we ambulate primarily on our hind limbs in an erect posture. That allows for many advantages in mobility, freedom of use for the upper extremities, an elevated perspective to survey our surroundings, and a higher profile to deter predators.
The downside — literally — is the potential for a much greater moment of force exerted on the trunk and upper body with a fall. Thus, a fall on the hip, ischium, sacrum, knee, or any other osseous structure not only alters bone size and shape locally (intraosseous injury), but it can also transmit significant forces into the fluid-filled pelvic basin, abdomen, and thorax.
The fluid in these compartments is relatively contained, and since it is mostly composed of water, it is essentially a dense, noncompressible substance. As such, it can only respond to impact with outward expansion, much in the way a water balloon will explode on impact with the ground. Thus, the outwardly directed force, in turn, transmits the effect of impact into the surrounding bony framework (pelvis, spine, rib cage, and even the cranial vault). This secondary injury (outgoing impact) only adds to the structural deformation of bone, not to mention the visceral fascia.
A New Understanding of Biomechanics at the Cellular Level
To make sense of the effects of injury in general, including pelvic injury, we also need to recognize the importance of the interconnected nature of the entire fascial framework of the body. This framework consists of macroscopic structures, such as the skeleton, myofascial elements, visceral fascia, and the newly recognized interstitium.5 At the microscopic level, it is comprised of the cytoskeleton and the extracellular matrix (ECM). 6, 7 This continuous intracellular and extracellular framework dictates that a mechanical force applied to one part of the body is immediately transmitted to every other part of the body.
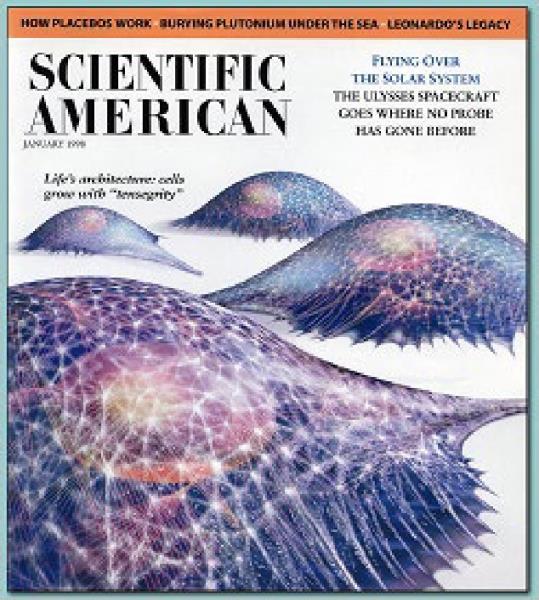 Figure 1: “The Architecture of Life,” D. E. Ingber, “Scientific American.
Figure 1: “The Architecture of Life,” D. E. Ingber, “Scientific American.
According to Dr. Donald Ingber, MD, PhD, a cellular biologist who has been investigating the mechanical and physiological properties of the cytoskeleton in great depth (Figure 1), the mechanical force of an injury alters the molecular elements of the cytoskeleton and the ECM from a flexible state to one that is enlarged and rigid, resulting in biomechanical, physiological, and biochemical changes.8 These local areas of restriction are, in turn, transmitted throughout the body, based on the principle of “tensegrity.” My understanding of the importance of this structural concept was further clarified through the work of Dr. Stephen Levin, MD, an orthopedic surgeon who coined the term “biotensegrity” to describe this revolutionary model of living tissue.9, 10
Connections: How Injury of the Bones of the Pelvis Causes Biomechanical Imbalance
Based on the interconnected nature of tissue, as described earlier, injury and subsequent enlargement/deformation of bone and the deeper layers of fascia associated with fluid-filled visceral organs (which I have defined as “primary restrictions”11) in structures such as the pelvis can alter the biomechanics of local and distant structures. This can result in strain, pain, reduced mobility, articular instability, and myofascial dysfunction in many other areas of the body (Figure 2). In the case of the pelvis, as previously outlined, this can include low back, hip and knee pain, and visceral dysfunction, such as incontinence, irritable bowel, dysmenorrhea, prostatitis, erectile dysfunction, and many other conditions.
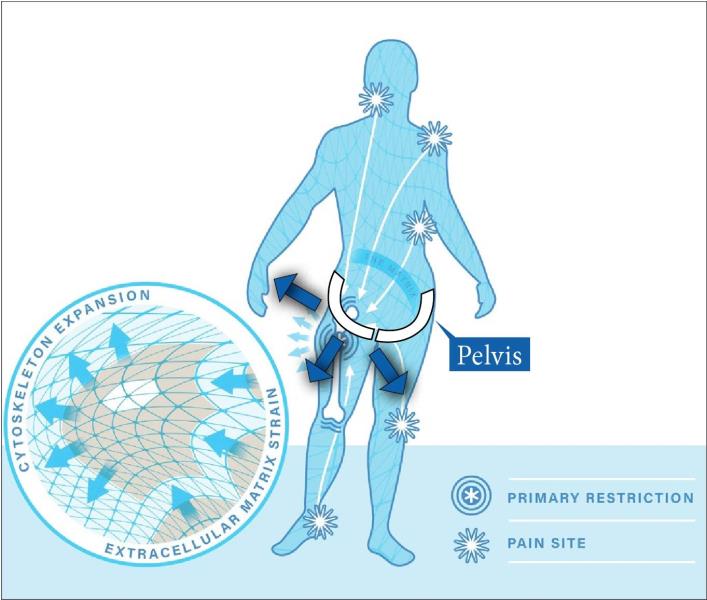 Figure 2: Injury patterns arising from a primary restriction in the pelvis, showing the transmission of mechanical tension to structures throughout the body, including strain at the level of the cytoskeleton and the extracellular matrix.
Figure 2: Injury patterns arising from a primary restriction in the pelvis, showing the transmission of mechanical tension to structures throughout the body, including strain at the level of the cytoskeleton and the extracellular matrix.
Treatment Solutions
Surprisingly, a gentle form of treatment applied directly to the involved osseous structure can almost instantly restore its normal size and shape. This dramatic transformation, which has been verified with radiographic evidence, takes advantage of the piezoelectric nature of bone.12, 13
The assessment process involves the identification of any primary restrictions accumulated over a lifetime. Treatment consists of gentle pressure combined with a normalizing magnetic field, which appears to allow the molecular structure of the cytoskeleton and the extracellular matrix to return to its preinjury state. This typically leads to a restoration of optimal biomechanical and physiological function, resulting in an improvement in overall well-being. Besides being able to apply this process to the pelvis, spine, rib cage, and extremities, its application to cranial trauma has been acknowledged by a leading expert in the field of traumatic brain injury.14
In summary, improving our understanding of the physics of injury within the deeper framework of the body, including the cellular and molecular levels, can allow us to provide better and more lasting solutions for our patients who are experiencing pelvic dysfunction and many other conditions.
References:
Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019 Jun;22(3):217-222. doi: 10.1080/13697137.2018.1543263. Epub 2018 Dec 21. PMID: 30572737.
Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36:104-13. doi: 10.1093/epirev/mxt009. Epub 2013 Nov 26. PMID: 24284871.
Leslie SW, Sooriyamoorthy T. Erectile Dysfunction. 2024 Jan 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32965924.
Benias PC, Wells RG, Sackey-Aboagye B, Klavan H, Reidy J, Buonocore D, Miranda M, Kornacki S, Wayne M, Carr-Locke DL, Theise ND. Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Sci Rep. 2018 Mar 27;8(1):4947. doi: 10.1038/s41598-018-23062-6. Erratum in: Sci Rep. 2018 May 10;8(1):7610. PMID: 29588511; PMCID: PMC5869738.
Fantner GE, Hassenkam T, Kindt JH, Weaver JC, Birkedal H, Pechenik L, Cutroni JA, Cidade GA, Stucky GD, Morse DE, Hansma PK. Sacrificial bonds and hidden length dissipate energy as mineralized fibrils separate during bone fracture. Nat Mater. 2005 Aug;4(8):612-6. doi: 10.1038/nmat1428. Epub 2005 Jul 17. PMID: 16025123.
Chen CS, Ingber DE. Tensegrity and mechanoregulation: from skeleton to cytoskeleton. Osteoarthritis Cartilage. 1999 Jan;7(1):81-94. doi: 10.1053/joca.1998.0164. PMID: 10367017.
Pischinger A. The Extracellular Matrix and Ground Regulation, Basis for a Holistic Biological Medicine. Berkley: North Atlantic Books, 2007.
Ingber DE. The architecture of life. Sci Am. 1998 Jan;278(1):48-57. doi: 10.1038/scientificamerican0198-48. PMID: 11536845.
Levin SM. The Importance of Soft Tissues for Structural Support of the Body. Spine: State of the Art Reviews . 1995 May;9(2).
Tadeo I, Berbegall AP, Escudero LM, Alvaro T, Noguera R. Biotensegrity of the extracellular matrix: physiology, dynamic mechanical balance, and implications in oncology and mechanotherapy. Front Oncol. 2014 Mar 4;4:39. doi: 10.3389/fonc.2014.00039. PMID: 24624363; PMCID: PMC3940942.
Roth GB. The Matrix Repatterning Program for Pain Relief. Oakland: New Harbinger Publications, 2005.
Chakkalakal DA. Mechanoelectric transduction in bone. Journal of Materials Research. 1989; 4, 1034–1046. doi: 10.1557/JMR.1989.1034
MacGuintie LA. Streaming and piezoelectric potentials in connective tissues, In: Blank M (ed). Electromagnetic fields: biological interactions and mechanisms. Advances in Chemistry Series 250. Washington DC: American Chemical Society; 1995.125-142p.
Doidge N, The Brain’s Way of Healing. New York: Penguin Books; 2015.
Dr. George Roth is a graduate of the University of Toronto, Canadian Memorial Chiropractic College and the Ontario College of Naturopathic Medicine and has studied osteopathic medicine at Doctors’ Hospital North, Columbus, Ohio. He is the developer of Matrix Repatterning and is the director of education at the Matrix Institute in Toronto. Dr. Roth has presented seminars at numerous hospital- and university-based symposia throughout North America. He is the coauthor with Kerry D’Ambrogio, PT, of Positional Release Therapy, and the author of The Matrix Repatterning Program for Pain Relief. His work is also featured in The Brain’s Way of Healing by Dr. Norman Doidge.
 View Full Issue
View Full Issue