Low Back Pain, Revisited
TECHNIQUE
By
George B. Roth
BSc, DC, ND
It’s been referred to as the scourge of modern man. The age-old affliction of low back pain has likely been with us since we achieved the upright posture. Over the millennia, healers and practitioners of all stripes have grappled with this challenging condition—stretching, pummeling, cracking, and even hacking to alleviate the pain and discomfort of this often debilitating condition. The challenge, of course, is that most of the approaches used throughout the healthcare system have failed to provide long-term solutions.
According to the American Chiropractic Association:
• Worldwide, [low] back pain is the single leading cause of disability, preventing many people from engaging in work as well as other everyday activities.
• It is one of the most common reasons for missed work. One-half of all working Americans admit to having back pain symptoms each year.
• It accounts for more than 264 million lost work days in one year—that’s two work days for every full-time worker in the country.
• Experts estimate that up to 80% of the population will experience low back pain at some time in their lives.
• [Low] Back pain can affect people of all ages,
• from adolescents to the elderly.
• It is the third most common reason for visits to the doctor’s office, behind skin disorders and osteoarthritis/joint disorders.
• Most cases of are mechanical or nonorganic— meaning they are not caused by serious conditions, such as inflammatory arthritis, infection, fracture, or cancer.
• Most people with low back pain recover but reoccurrence is common and, for a small percentage of people, the condition will become chronic and disabling.
• Worldwide, years lived with disability caused by low back pain have increased by 54% between 1990 and 2015.
• Low back pain costs Americans at least $50 billion in healthcare costs each year. Add in lost wages and decreased productivity, and that figure easily rises to more than $100 billion.
Adapted from the ACA Website
In this article, I would like to present some revolutionary concepts, which may help explain some of the underlying causes of low back pain, and by extension, many other painful biomechanical disorders. I hope to shed light on why some of the approaches currently in use may be helping—or not. This information is based on some of the latest scientific evidence of how the body is constructed at the cellular and molecular level. I believe a better understanding of how the body responds to injury, at the most fundamental level, may provide us with the insights necessary to offer real and lasting solutions.
When Physics Meets Biology
I often begin my presentations to practitioners and the public with the following request, “Put up your hand if you’ve never had a fall.” So far, no takers.
Walking the earth on two legs has provided us with tremendous advantages: freeing the upper extremities to be able to manipulate the environment (gather food, wield tools and weapons); presenting a higher profile to deter predators; and the ability to survey our surroundings for potential threats and opportunities. However, one of the main trade-offs is that the upright, bipedal posture has made us more vulnerable to the laws of physics—namely gravity, inertia, and momentum.
As a result of this vulnerability, we begin the assault on our bodies at a fairly young age. From the moment we set forth on two toddling legs, this often takes the form of slipping and falling on the ground or the stairs, bumping into furniture, tripping over toys, and bumping our heads on cupboards, door frames, and our siblings. As we get older, we tend to engage in activities that put us at further risk for injury, such as high-speed and contact sports, motor vehicle collisions, etc. The list goes on and on.
The Importance of Density
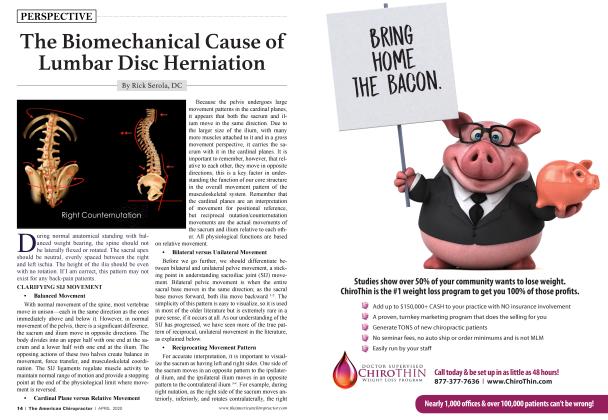
Although all parts of the body are biomechanically interconnected via the extracellular matrix and the cytoskeleton (Figure 1a, 1b above), certain areas are more vulnerable to injury due to their inherent structure. Simple physics tells us that a structure with a higher density will absorb the force of an injury to a greater degree than another structure with a lower density. For example, if you strike a pillow with a hammer, there will be practically no sound and little or no evidence of the assault, given that the force is easily dissipated by the loosely arranged structural elements of the filling material. In contrast, striking a piece of wood, such as a tabletop, will make a lot of noise, since the more closely packed molecules will bounce off of each other, setting the surrounding air molecules in motion, which cause the eardrum to vibrate more vigorously. As a result of its greater density, the wood will clearly and permanently demonstrate the effects of the “injury.”
One of the densest substances on the planet is water. For this reason, a water-filled balloon tends to explode on impact with the ground because water is considered a noncompressible substance since its molecules are tightly packed together. Water, in various forms (blood, lymph, cerebrospinal, and other serous fluid components), constitutes a significant proportion of the human body. Therefore, impact injuries tend to primarily be absorbed by the fluid-filled areas of the body in the torso (internal organs) and the cranium. These fluid-filled areas will rapidly expand on impact, transferring the force to the surrounding structures.
Another dense substance is bone, which is a form of mineralized fascia. In a recent article (“Is It Time for Chiropractic to Evolve?” The American Chiropractor, December 2019), I presented evidence that bone expands with injury (Figure 2)5. My theory is that these changes in bone size, especially in the spinal area, might appear as misalignment (subluxation), when, in fact, evidence suggests that this is most likely due to asymmetrical enlargement of one portion of a vertebral segment or segments. Radiological and anatomical investigation appears to support this contention.
Noticing Changes in Bone Size:
A simple inspection of a skeletal model, cast from an actual specimen, will reveal many of these asymmetries (spine, humerus, femur, tibia, etc.). Detecting and correcting these injuries, has been the focus of my work and what I have taught to practitioners for almost 30 years. If you take the time to measure the width of each of your knees at the distal epiphysis of the femur, or the patella, you will likely note a difference. It may prompt a long-forgotten memory of that time you fell on your knee. With some of your patients, observing the relative size of the proximal head of the humerus, the scapula, or the grater trochanter on one side versus the other will provide you with some additional confirmation of these differences. Further evidence may also be apparent if you inspect the shape of the skull and note asymmetrical areas of depression or expansion in the cranial vault.
It may be valuable to note that the side of expansion of the occipital and temporal bone is often accompanied by the relative prominence of the upper cervical spine on the same side. My contention is that the appearance of a so-called rotation of Cl or C2 is, in fact, an expansion of the articular process on that side. In addition to direct injuries to bone, impact injuries to the fluid-filled compartments of the body are transferred to their boney protective surroundings, such as the rib cage, spine, pelvis, and cranium. In a sense, every impact to the body is two impacts-one incoming and one outgoing-due to the transfer from the fluid-filled trunk or cranium to the surrounding osseous framework.
The Role of Stability
In a previous article (“Solutions for Low Back Pain and Instability,” February 2017), I referred to the articular stability reflex (ASR), a mechanism I discovered in the mid-1990s, which appears to explain how the loss of stability in certain joints may contribute to the development of pain and articular degeneration. Muscles, which provide dynamic stabilization, such as the popliteus and medial hamstrings (knee), supraspinatus (shoulder), gluteus medius (hip), tibialis anterior (ankle), and multifidus and rotatores (lower lumbar spine), are literally turned off in response to certain injuries. I speculated that this mechanism would have the effect of mitigating the transfer of additional strain to core structures, including the spinal cord, by creating a “wobble zone” these peripheral joints, which I refer to as sacrificial joints. It is important to note that the spinal cord is not present in the lower lumbar spine, which might explain why it is also sacrificed, so to speak.
Programs to develop “core strength” have been promoted to counteract this response; however, it is my contention that it is not possible to strengthen these particular muscles because they are essentially denervated, i.e., turned off. This would be like repeatedly changing a light bulb in a lamp that is unplugged in an attempt to make it work.
The resultant instability may play a role in the degeneration of those structures by increasing mechanical stress on articular cartilage, menisci, subtending bone, and the intervertebral disc, in the case of the lower lumbar spine. These observations have been validated by recent evidence 1-4 Our experience has demonstrated that treatment of the underlying structures, which initiate the ASR, tends to immediately reestablish normal tone and function of the stabilizing muscles, literally restoring joint stability, like turning on a light switch.
Possible Mechanisms Leading to the Development of Low Back Pain
Low Back Pain - an Accident Waiting to Happen
In the illustrations (above), the diagram on the left (Figure 3) represents the ideal structural balance of the skeletal components of the lower quadrant and normal tone of the stabilizing elements of the spine (intrinsic intervertebral musculature). The diagram on the right (Figure 4), illustrates several structural imbalances, including relative enlargement of the right femur and innominate, ipsilateral enlargement of the right side of the sacrum, L4, 5, and depression of the right lower ribs along with ipsilateral enlargement of the associated vertebra. These injuries are commonly observed subsequent to a fall on the side. This will typically result in hypertonicity of several myofascial elements, including the iliopsoas, quadratus lumborum, gluteus, and the iliotibial band. By contrast, the lower lumbar paraspinal intrinsic muscles (dynamic stabilizers) tend to become relatively hypotonic as part of the articular stability reflex response (see above).
These, and many other common injuries, are often associated with similar structural and functional changes. Once these imbalances develop, the mechanical stress imposed on the lower lumbar discs and other articular elements begins the chronic, degenerative decline toward annular deterioration, inflammation, arthrosis, stenosis, and their associated neurological consequences.
Summary
Our assumptions about the causes of many structural conditions, including low back pain, may need to be revisited in light of new revelations about the underlying structure of the body and how it responds to injury at the most fundamental level. Our understanding of the consequences of physical trauma in the form of impact or strain has evolved significantly in the past 50 years, and it is essential that we adapt our clinical interventions to incorporate these discoveries. We owe it to ourselves and our patients to strive to achieve the lasting and profound solutions that are now within our grasp.
References:
1. Reinold MM, et al, Electromyographic Analysis of the Supraspinatus and Deltoid Muscles During 3 Common Rehabilitation Exercises, Journal of Athletic Training, 2007; 42(4): 464-469.
2. Fibre type characteristics and function of the human paraspinal muscles: normal values and changes in association with low back pain, Mannion AF, J Electromyog. Kinesiol. Dec 1999, 9 (6): 363-77.
3. Atrophy of sacrospinal muscle groups in patients with chronic, diffusely radiating lumbar back pain, Laasonen EM, Neuroradiology. 1984;26:9-13
4. Electromyographic Study of the Popliteus Muscle in the Dynamic Stabilization of the Posterolateral Corner Structures of the Knee, K Schinhan, et al, Am J Sports Med, Vol. 39, no. 1, 173-179, January, 2011.
5. Fantner GE, Hassenkcim T, Kindt JH, Weaver JC, Birkedal H, Pechenik L, Cutroni JA, Cidade GA, Stucky GD, Morse DE, Hansma PK, Sacrificial bonds and hidden length dissipate energy as mineralized fibrils separate during bone fracture, Nat Mater. 2005 Aug; 4(8): 612-6. Epub 2005 Jul 17.
6. Roth GB, The Matrix Repatterning Program for Pain Relief, New Harbinger Publications, Oakland, CA, 2005.
7. A New Evaluation Method for Lumbar Spinal Instability: Passive Lumbar Extension Test, Kasai Y, Morishita K, Kawakita E, Kondo T, Uchida A, JAPTA, December 2006.
8. Lumbar instability: an evolving and challenging concept, Beazell JR, Mullins M, Grindstaff TL, J Man Manip Ther, 2010 Mar; 18 (1): 9-14
9. Function of the Supraspinatus Muscle and its Relation to the Supraspinatus syndrome - An Experimental Study in Man, B Van Linge, JD Mulder, Journal of Bone and Joint Surgery, Vol 45B, No. 4, November 1963, pp 750-754.
Dr. George Roth has been practicing as a chiropractor and a naturopathic physician for 40 years. He has taught at chiropractic, naturopathic, medical, osteopathic, physical therapy, and medical schools throughout North America. He is the coauthor, with Kerry D'Ambrogio, PT, of Positional Release Therapy (Elsevier, 1997), and the author of The Matrix Repatterning Program for Pain Relief (New Harbinger, 2005). His work is also featured in The Brain's Way of Healing by Dr. Norman Doidge (Penguin, 2016). For more information, visit matrixforpractitioners.com.
 View Full Issue
View Full Issue