DURING MY 44 YEARS OF PRACTICE, I have utilized many tools, both diagnostic and therapeutic. However, no tool has had a greater impact on the success of my practice than manual muscle testing.
Unfortunately, when most chiropractors hear the words “manual muscle testing,” they equate them with two other very intimidating words, namely “applied kinesiology.” Their thoughts quickly shift to, “I wonder what we’re having for supper...” As a result, this valuable technique is overlooked or ignored completely in their practice.
We all have some similar and different tools in our toolboxes. However, we should all have the adjustment in common. Manual muscle testing provides immediate feedback to the doctor and the patient that something was accomplished on that visit. Otherwise, when the patient’s family and friends ask about their experience in our office, they will say something such as, “He cracked my neck and shined this red light on me,” or, “He used this little clicker thing on my neck, but I’m not sure what that did!”
I have listened to patients describe their experiences in other DC offices for over four decades. They simply do not understand why we do what we do. When they see an immediate change in muscle strength or range of motion, though, they know that we have changed something in their spine.
Even if their pain wasn’t completely alleviated, they are on the road back to recovery. “When I went in, I couldn’t lift my arm, but when I left, I had a lot more strength in my arm and shoulder,” is a much better testimonial than, “He cracked my neck on both sides and told me to come back three times a week to do it again.”
One of my main critiques of chiropractic education today and when I was in college is the disconnect between diagnostic training and connecting that training with the clinical application of a chiropractic adjustment. Can anyone truthfully say if any of the countless ortho and neuro tests that we were forced to memorize and perform on patients and for board exams were beneficial in obtaining a specific listing and level of a vertebral subluxation? Do positive Nachlas and Ely’s tests indicate whether to adjust the involved sacroiliac joint as a PUN or an ASEX, or is the real issue the sacrum? It’s anybody’s guess.
We were required to purchase Dr. Stanley Hoppenfeld’s Orthopaedic Neurology: A Diagnostic Guide to Neurologic Levels. In that book, Dr. Hoppenfeld organized a very systematic approach for determining the level of neurological insult to the nervous system by utilizing three basic tools — pinwheel exam, reflex testing, and manual muscle testing.
“However, manual muscle testing provides a clearer indication of whether a problem may originate in the spine or locally.”
I will admit that after all my years in practice, I still find it difficult to get an accurate read using reflex hammer testing, not to mention the unpleasant sensation from whacking my tender aging thumbnails with that blasted hammer. Pinwheel examination presents its own set of variables because it involves a subjective assessment of the test by the patient.
However, manual muscle testing provides a clearer indication of whether a problem may originate in the spine or locally. It provides the added benefit of giving the doctor and patient immediate feedback about the effectiveness of the treatment, namely the adjustment.
Let’s create a hypothetical clinical scenario and see how we can connect the dots between our assessment and our adjustment. A patient presents with a complaint of neck pain radiating into his right shoulder and arm that began after working on “a little home project” involving concrete. However, his “little home project” involved digging with a pick and shovel, raking with a hoe, building forms for the concrete (hammer!), lifting 80 lb. bags of concrete, mixing the concrete (more raking!), and then shoveling the concrete into the prepared forms.
Upon examination with manual muscle testing, you find weakness of the right deltoid and biceps relative to the left. You instruct the patient to flex his neck, and then you retest the weak muscles. You repeat the test with the patient’s neck in extension, right and left rotation, and right and left lateral flexion. You find that his strength improves with cervical extension, left lateral flexion, and left rotation. Obviously, these neck positions relieve some of the irritation to the C5 nerve root and might come into play when deciding in which position(s) to place the patient’s neck when delivering the adjustment.
Then, you decide to take things one step further. You instruct the patient to place his left middle finger on the left side of the C5 spinous process and apply a slight left-to-right pressure on the vertebra while you retest the previously weak muscles. You then do the same as he applies right-to-left pressure on the C5 spinous process by hooking his left middle finger on the right side of the C5 spinous process and pulling the spinous to the left.
This time, the weak muscles strengthen with left-to-right pressure on the spinous process. So now you have determined that your listing is roughly a PL for a spinous contact or a PL-L for a lamina contact, and that you will deliver the adjustment with the patient’s cervical spine in slight extension and left rotation. This would most likely involve a contact on the right lamina of C5. You could then take a left spinous contact and deliver your thrust with the patient’s neck in left lateral flexion.
Upon retesting the weak muscles after the adjustment, you find that both muscles have greatly improved in strength. You and your patient know with certainty that your adjustment immediately changed their physiology. It doesn’t matter whether you use an instrument to deliver the thrust or your hands. The outcome will be the same.
If you want to take things further, you can add any number of ancillary procedures. You can use a cold laser on the C5 nerve root and directly on the involved muscles. If you are an A-K doctor (like me), you can treat the neurolymphatic and neurovascular reflexes for the involved muscles. You can perform some myofascial release or apply your percussor to the muscles.
You may ask, “How can utilizing this technique enhance my practice when it will involve spending more time with each patient?” I can test all the upper and lower extremity muscles in less than a minute per region and come very quickly to a decision on what my adjustive and adjunctive procedures will be on that particular visit.
As a result, I have moved my practice away from the musculoskeletal-oriented practice I had in my early years to a more holistic health-oriented practice. Today’s patients are much more knowledgeable about health and are in search of doctors who can keep them healthy without medications.
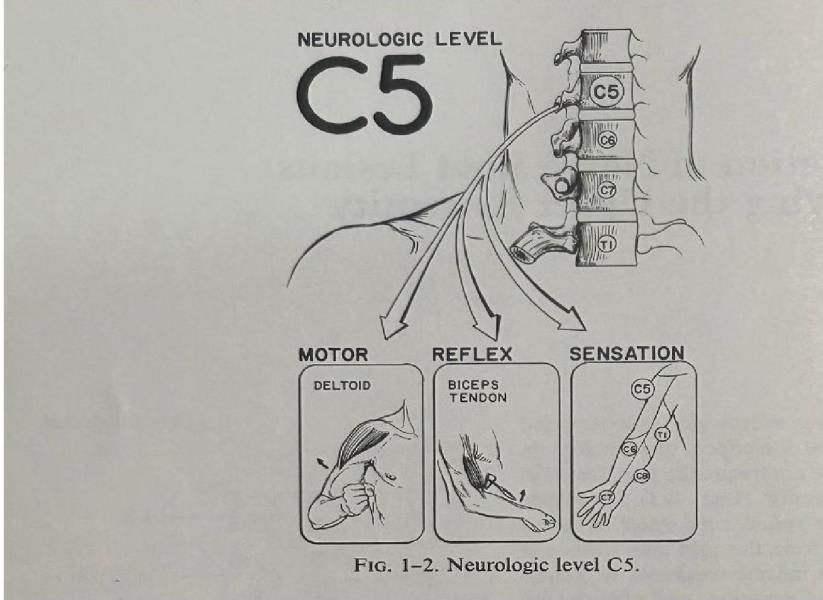 Evaluation of Nerve Root Lesions Involving the Upper Extremity
Evaluation of Nerve Root Lesions Involving the Upper Extremity
They don’t want to end up like their parents on a dozen or more prescription drugs with high blood pressure, diabetes, and dementia.
I have also learned that if we want to be taken seriously by the public, then we must take what we do in our offices a little more seriously. Invest some time in reviewing the major muscles relating to the various neurological levels in the cervical and lumbar spines. Then, relearn how to test those muscles correctly and quickly. When a weakness is found, take that region of the spine through its six basic ranges of motion to determine which position is best for delivering the adjustment. From that starting point, you can then learn the muscle-organ relationships described by Goodheart to begin adding nutritional testing to your toolbox.
I encourage you to take that copy of Hoppenfeld’s book off your shelf, dust it off, and start reviewing your basic neurology. Then, purchase a copy of David Walther’s Synopsis and start learning how to add the neurolymphatic and neurovascular reflexes to your toolbox. After that, you’ll be ready to add the organ reflexes, and your practice life will never be the same again.
I have developed a muscle-testing technique involving the acupuncture meridians that I have used successfully for the past 25 years to build a substantial nutritional side to my practice. The meridians provide valuable insights into how organ stresses are referring to the spine and contributing to recurring vertebral subluxations. In future articles, I will describe the development of my viscero-somatic reflex technique (VSRT) and how manual muscle testing can be taken to the next level. Now get to work!
Dr. John Wohar graduated Summa Cum Laude from Palmer College of Chiropractic in Davenport, Iowa in 1981. He and his wife, Linda, are the proud parents of 10 children and 20 grandchildren. He practices now from his home office in California, Pennsylvania, where he continues to develop his viscero-somatic reflex technique. He can be reached at [email protected].
References
1. Hoppenfeld S, Hutton R. Orthopaedic Neurology : A Diagnostic Guide to Neurologic Levels. Philadelphia: Lippincott; 1977.
 View Full Issue
View Full Issue