Spinal discs play a crucial role in the lower back, serving as shock absorbers between the vertebrae, supporting the upper body, and allowing a wide range of movement in all directions. As we focus on disc disease, our goal as chiropractors is for all doctors to know the causes and treatments.
The fact is a subluxation can progress to a bulge, which can progress to a herniation. If the herniation sequesters, the pain and symptoms will progress. According to the studies of Drs. Martin and Boxell of the Department of Neurological Surgery, University of Oklahoma, Oklahoma City; and the Oklahoma Spine and Brain Institute, Tulsa, Oklahoma, “Lumbar disc degeneration occurs commonly in humans. There are a variety of factors that contribute to this condition. The disc itself is active tissue that contains significant mechanisms for self-repair.”
Their study also states, “The lumbar discs most often affected by degeneration that leads to herniation are L4-5 and L5-S1, most probably because of a combination of longstanding degeneration and a subsequent change in the ability of the disc to resist applied stress. Discs that are degenerated show abnormal vascularity, and abnormal distribution of collagen and collagen crosslinks. They also show an abnormal and nonuniform elastic modulus that distributes stress to critical portions of the disc. Radicular pain is often associated with disc herniation, which may be due, in part, to an inflammatory response to the portion of nucleus that has been extruded.”
The key to the above study indicates evidence that the disc has the ability to repair itself. As a chiropractor, I’ve always believed that the power that creates the body has the power to heal the body; therefore, surgical interventions should be the last and final resort, which is why Nonsurgical Spinal Decompression is the future of our profession.
Let’s review the basics. If a disc herniates and leaks some of its inner material, the disc can quickly go from easing daily life to aggravating a nerve, triggering back pain, and possibly causing pain and nerve symptoms down the leg.
Disc herniation symptoms usually start for no apparent reason; or, they may occur when a person lifts something heavy and/or twists the lower back, motions that put added stress on the discs.
A herniated disc refers to a problem with one of the rubbery cushions (discs) that sit between the individual bones (vertebrae) that stack to make your spine.
A spinal disc has a soft, jelly like center (nucleus) encased in a tougher, rubbery exterior (annulus). In the past a non-medical term referred to this as a slipped disc. It actually does not slip, it herniates. A herniated disc occurs when some of the nucleus pushes out through a tear in the annulus. A herniated disc, which can occur in any part of the spine, most commonly cervical and lumbar, can irritate a nearby nerve causing symptoms. Depending on where the herniated disc is, it can result in pain, numbness, or weakness in an arm or leg.
Many studies indicate that cervical and lumbar herniated discs are a widespread medical problem, most often affecting people between the ages of 35 to 50. Additional studies indicate surgery may not be the answer.
Research clearly shows that disc herniation is most often the result of gradual, aging-related wear and tear called disc degeneration. As you age, your discs become less flexible and more prone to tearing or rupturing with even a minor strain or twist, which is why athletes and active people are prone to generative disc disease, DDD. Because the disc consists of 87% fluid, we are able to rehydrate the disc with NSSD. Dr. Richard Lohr, President of the International Disc Education Association (IDEA), states that using NSSD is like, “milking the disc, bringing fluid and nutrients back into the disc, preventing the disc from collapsing.”
Many patients come to your office who can’t pinpoint the source of their herniated disc. Sometimes, simply using back muscles instead of leg and thigh muscles to lift heavy objects can lead to a herniated disc, as can twisting and turning while lifting. We know that prevention comes before rehabilitation.
When pressure or stress is placed on the spine, the disc’s outer ring, the annulus, may bulge, crack, or tear. If such an injury occurs in the lower back (the lumbar spine), the disc protrusion may push against the nearby spinal nerve root, and the inflammatory material from the interior may then irritate the nerve. The result is shooting pains into the buttock and down the leg. We have found that laser treatment helps the annulus heal.
A tough outer ring called the annulus protects the gellike interior of each disc, known as the nucleus pulposus. Due to aging and continual wear and tear, the discs lose some of the fluid that makes them pliable and spongy. As a result, the discs tend to become flatter and harder. This process—known as disc degeneration—can start early in life, which often shows up in imaging tests in early adulthood, which is why an MRI is so important. Remember, a subluxation can become a bulge, and a bulge can become a herniation
Factors that can increase a patient’s risk of a herniated disc include:
• Weight. Excess body weight causes extra stress on the discs in your lower back.
• Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways, and twisting also can increase your risk of a herniated disc.
• Genetics. Some people inherit a predisposition to developing a herniated disc.
• Smoking. It’s thought that smoking lessens the oxygen supply to the disc, causing it to break down more quickly.
• Just above your waist, your spinal cord ends. What continues through the spinal canal is a group of long nerve roots that resemble a horse’s tail (cauda equina). The goal is to catch DDD before the progression of cauda equina syndrome. In some cases disc herniation can compress the entire spinal canal, including all the nerves of the cauda equina. This condition can lead to foot drop, loss of bowel function, and possible emergency surgery, which may be required to avoid permanent weakness or paralysis.
We see more herniated discs in the lower back, although they can also occur in the neck. Signs and symptoms depend on where the disc is situated and whether the disc is pressing on a nerve. They usually affect one side of the body.
• Arm or leg pain. If your herniated disc is in your lower back, you’ll typically feel the most pain in your buttocks, thigh, and calf. You might have pain in part of the foot, as well. If your herniated disc is in your neck, you’ll typically feel the most pain in your shoulder and arm. This pain might shoot into your arm or leg when you cough, sneeze, or move into certain positions. The pain is often described as sharp or burning.
• Numbness or tingling. People who have a herniated disc often have radiating numbness or tingling in the body part served by the affected nerves.
• Weakness. Muscles served by the affected nerves tend to weaken. This can cause you to stumble or affect your ability to lift or hold items.
Some patients may have a herniated disc without any symptoms. You might not know how severe it is unless it shows up on a spinal image. Therefore, imaging is very important in making the right diagnosis.
To help prevent a herniated disc we teach our patients to do the following:
• Exercise. Strengthening the trunk muscles stabilizes and supports the spine.
• Maintain good posture. This reduces pressure on your spine and discs. Keep your back straight and aligned, particularly when sitting for long periods. Lift heavy objects properly, making your legs — not your back — do most of the work.
• Maintain a healthy weight. Excess weight puts more pressure on the spine and discs, making them more susceptible to herniation.
• Quit smoking. Avoid the use of any tobacco products.
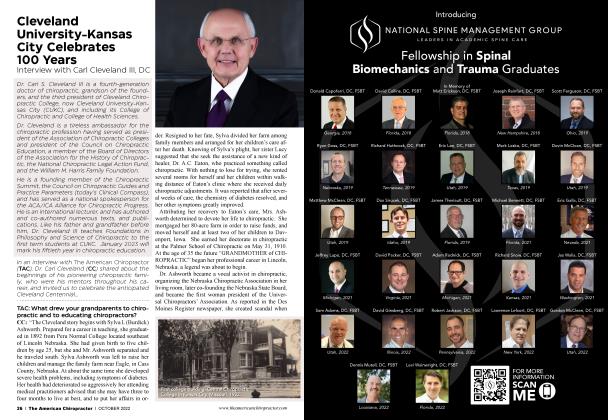
During 34-plus years as business partners, Dr. Eric Kaplan and Dr. Perry Bard have developed Disc Centers of America, Concierge Coaches, and the first national certification program for non-surgical spinal decompression a 12 CEU credit event. Being held for the 10th anniversary on November 5,6. This event has been sold out for two years running.
Dr. Jason Kaplan is a Parker University graduate practicing in Wellington, Florida with his wife, Dr. Stephanie Kaplan. Jason also is an Instructor for Disc Centers of America and teaches techniques for the National Certification Program at Life University. To learn more, call 888-990-9660 visit thechiroevent. com or decompressioncertified.org.
References
1. M. D. Martin, C. M. Boxell, and D. G. Malone Adams MA, McNally DS, Dolan P: ‘Stress ’ distributions inside intervertebral discs. The effects of age and degeneration. J Bone Joint SurgBr 78:965-972, 1996
2. Antoniou J, Goudsouzian NM, Heathfield TF, et al: The human lumbar endplate. Evidence of changes in biosynthesis and de-naturation of the extracellular matrix with growth, maturation, aging, and degeneration. Spine 21:1153-1161, 1996
3. Antoniou J, Steffen T, Nelson F, et al.: The human lumbar inter-vertebral disc: evidence for changes in the biosynthesis and de-Neurosurg. Focus / Volume 13 August, 200 Pathophysiology of lumbar disc degeneration naturation of the extracellular matrix with growth, maturation, ageing, and degeneration. J Clin Invest 98:996 1003, 1996
4. Bartels EM, Fairbank JC, Winlove CP, et al.: Oxygen and lactate concentrations measured in vivo in the intervertebral discs ofpatients with scoliosis and back pain. Spine 23:1-8, 1998
5. Blain EJ, Gilbert SJ, Wardale RJ, et al.: Up-regulation of matrix metalloproteinase expression and activation following cyclical compressive loading of articular cartilage in vitro. Arch Bio-chem Biophys 396:49-55, 2001
6. Bogduk N: The anatomy of the lumbar intervertebral disc syndrome. MedJAust 1:878-881, 1976
7. Bogduk N, Tynan W, Wilson AS: The nerve supply to the hu-man lumbar intervertebral discs. JAnat 132:39-56, 1981
8. Brisby H, Balague F, Schafer D, et al: Glycosphingolipid anti-bodies in serum in patients with sciatica. Spine 27:380-386, 2002
9. CoppesMH, Marani E, Thomeer RT, et al: Innervation of “painfid” lumbar discs. Spine 22:2342-2350, 1997
10. Crock HV, Goldwasser M: Anatomic studies of the circulation in the region of the vertebral end-plate in adult Greyhounddogs. Spine 9:702-706, 1984
11. Doita M, Kanatani T, Harada T, et al: Immunohistologic study of the ruptured intervertebral disc of the lumbar spine. Spine21:235 241, 1996
 View Full Issue
View Full Issue