Chronic pain is defined as pain that has persisted for more than three months. According to the CDC, chronic pain has been linked to numerous physical and mental conditions and contributes to high health care costs and lost productivity. A limited number of studies estimate that the prevalence of chronic pain ranges from 11% to 40%. In 2016, an estimated 20.4% ofU.S. adults (50.0 million) had chronic pain.1
As chiropractors, we have all had patients with chronic pain. Pain is the number one reason patients seek our care and one of our first tasks is to try to determine the contributing factors that are causing pain. The most common and likely cause of chronic pain is previous trauma and degenerative arthritis. Other common causes of chronic pain include cancer and neurogenic pain from neuropathy. The chiropractic office is not usually the first place patients have sought solutions for their pain as many have already been treated in clinics that
According to the CDC, chronic pain has been linked to numerous physical and mental conditions and contributes to high health care costs and lost productivity.
specialize in pain management. The fact that they are still seeking relief is indicative of the difficulty that treating chronic pain can present. Countless methods, remedies, drugs, and procedures have been created, and all have limited benefits and effectiveness.
Brain Chemistry
According to Harvard Medical School, pain is depressing, and depression causes and intensifies pain. People with chronic pain have three times the average risk of developing psychiatric symptoms — usually mood or anxiety disorders — and depressed patients have three times the average risk of developing chronic pain.
Brain pathways that handle the reception of pain signals, including the seat of emotions in the limbic region, use some of the same neurotransmitters involved in the regulation of mood, especially serotonin and norepinephrine. When regulation fails, pain is intensified along with sadness, hopelessness, and anxiety. And chronic pain, like chronic depression, can alter the functioning of the nervous system and perpetuate itself.2
It’s a complex problem that seems to be getting worse. I have noticed in my own practice that more and more patients are reporting high levels of anxiety and depression, and some are even suffering with suicidal ideations.
A report published by the World Health Organization (WHO) states that in the first year of the COVID-19 pandemic, the global prevalence of anxiety and depression increased by a massive 25%. The changes in brain chemistry can magnify how one experiences pain, making it that much more difficult to treat. Even with the pandemic now behind us, many are still suffering from the complexity of the combination of physical pain and effect of anxiety.3
This can contribute to chronic pain that’s not tied to an injury or physical illness. Psychogenic or psychosomatic pain is caused by psychological factors such as stress, anxiety, and depression. Many scientists believe this connection comes from low levels of endorphins in the blood.
The past several years have shown us the devastating effects of the opioid crisis when drugs are used for the treatment of chronic pain. According to the National Center for Drug Abuse Statistics, more than four times as many people died from drug overdose (OD) than from homicide in the first month of 2021 4
• 96,779 drug overdose deaths were reported from March 2020 to March 2021 which was 36.1% higher than the previous annual high from December 2018 to December 2019 (71,130 deaths).
• Preliminary reports indicate the number of drug overdose deaths in America increased 29.6% in 2020 and in January 2021, drug overdose deaths exceeded homicides by 306.7%.
The use of opioids for the treatment of chronic pain has been disastrous! The medical approach to chronic pain almost always includes the use of prescription drugs including anticonvulsants for nerve pain, antidepressants, corticosteroids, muscle relaxers, nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen. Topical products that contain pain relievers such as CBD or ingredients that create soothing heat or cold, TENS, nerve blocks and epidural steroid injections are other options commonly used, but they don’t address the cause of the pain, only the symptom.
It’s easy to be critical of the way pain is treated in this country, but the reality is that is can be a very complex problem made more complex by the limitations of the things we can influence in the way of patient compliance, lifestyle, diet, and exercise, or lack thereof There are solutions, but they can take time. It is often said, “people change, just not very much”. That can be the crux of the matter.
Contributors to chronic pain
When we have patients with chronic pain, the first step is to determine the causes of pain and the things that may be contributing to the pain mechanisms. As chiropractors, we may have a “slight” prejudice toward looking at biomechanical factors. This is infinitely important, because for all intents and purposes, we are the only healthcare providers looking at these things!
Sadly, many patients will be trapped in the cycle of seeking relief from chronic pain because of the duration of the conditions and the resultant adaptations that have resulted. I often tell patients who have long-standing, pain-producing arthritis and degeneration that “you can’t unboil a hard-boiled egg, but you can stop cooking it!” What does that mean? Even in the presence of chronic degenerative conditions that may or may not be related to trauma or disease, there are factors we can address that can improve their body’s ability to adapt, down regulate the stress chemicals that contribute to pain and potentially improve their quality of life.
Chronic Inflammation
Volumes of books and thousands of papers have been written on the effects of dietary inflammation on the human body. I will not belabor this point, but inflammation at the cellular level is significant in all of our patients because the American diet is loaded with inflammatory food components. Our body is constantly making new cells, but the fatty acid building blocks of cell membranes are predominantly made from inflammatory omega 6 fatty acids. This creates a myriad of biomechanical processes that drives pain, autoimmune responses, brain fog, leaky gut syndrome, anxiety, and depression.
I have seen patients make dramatic swings in their chronic pain levels from balancing out the omega 6 and omega 3 ratios by improving their diet and taking supplements. One dramatic case involved a young lady who was raised as a vegetarian and had an omega 6:3 ratio of 95 to 1. The nonnal ratio is 3:1. With changes in food choices and supplemental omega 3 fatty acids, her ratio returned to 3:1 in 6 months and her chronic pain was eliminated. We cannot overlook the importance of dietary inflammation, but it requires more than just adding supplements; fundamental changes must take place in the diet.
Posture and Movement
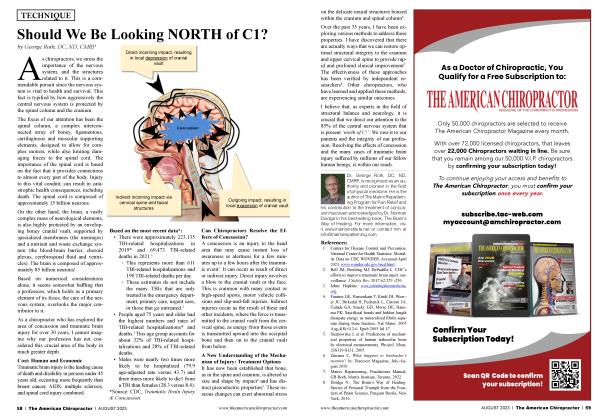
Biomechanical stress in the joints of the axial skeleton and spine can be drivers of pain and stimulation of the sympathetic nervous system because of the firing of nociceptive nerve fibers. This is the basis of what makes chiropractic effective because our care increases the firing of the proprioceptive fibers by our adjusting techniques which inhibits pain and enhances the reflexes associated with posture and joint movement.
I begin my search for biomechanical pain production in the foundation of the body, the feet. My experience includes measuring navicular drop in the feet of all of my patients for the first 15 years of my practice at which time, foot scanning technology was made available. Both methods have shown me that virtually all of my patients have an asymmetrical pedal foundation that creates small biomechanical distortions in the feet, knees and hips which then affect the pelvis, spine, and upper extremities. The effects of these distortions are cumulative over the years and are often overlooked until the compensatory responses begin creating symptoms. Degeneration in the knees, hips and spine are ubiquitous in our practices and go hand in hand with chronic pain.
In the study, “Effect of an orthotic intervention on sensorimotor integration mechanisms in patients with musculoskeletal disorders”, it reports that there is a preferred posture and movement pattern that is programmed into our DNA.5 Any posture or movement pattern that is less than optimal forces the body into compensatory patterns that become hard-wired neural networks, forcing the body to perform in suboptimal ways, which cause the chronic inflammatory and degenerative changes we see in the spine and extremities.
This is a fundamental cause of chronic pain, and we can help the patient develop strategies to return to more optimal posture and movement patterns and those strategies include chiropractic adjustments, custom flexible orthotics that support all three arches of the foot, specific exercises to restore preferred posture and functional movement patterns. This is part of the solution to helping the patient end their chronic pain and it is the strategy to prevent chronic pain from developing in the future.
Soft Tissue Sources
The myofascial system can also be a source of chronic pain. Older injuries from muscle strains that created scar tissue, myofascial dysfunction and trigger points can be addressed with low-tech mechanical devices. Compressing and lengthening the tissue with roller devices for muscle management improves the compliance of the muscle tissue and immediately creates an improvement in flexibility. Low Level Laser Therapy or Cold Laser has also been successfully used to address some of these soft tissue problems. Once the muscle and myofascia has regained its compliance, the ability to contract and relax, joint function begins to improve and the physiology of the joint returns to a healthier state.
Instrument Assisted Soft Tissue Mobilization (1ASTM) is a popular method for addressing myofascial restrictions. There are numerous devices available from handheld scraping tools to mechanical percussive tools with myofascial attachments as well as functional taping systems. 1 personally prefer the mechanical advantage of a percussive tool purely for the time savings it gives me. The textbook, “Anatomy Trains”, is a great resource that explains the superficial myofascial system and how to address it clinically.
Outside of the medical model for treating chronic pain, chiropractors have access to a significant arsenal of tools that assist the patient in restoring preferred posture, functional movement and reducing or eliminating chronic pain. In my personal practice, I use custom flexible orthotics to block the distortion patterns associated with asymmetrical foot pronation patterns. This creates a better proprioceptive response for balance and movement and decreases the nociceptive input that contributes to pain.
I utilize long axis spinal decompression to “stop cooking” the “hardboiled egg” of spinal degeneration. Cold laser therapy has been a fabulous technology to address joint and muscle pain with no side effects or toxicity. Whole body vibration in conjunction with specific preferred posture positioning helps patients regain functional movement patterns and posture. Nutritional guidance is essential in getting in front of the cellular and physiological components to chronic pain.
We have great tools and skills to help the chronic pain patient, but we are also virtually alone in the healthcare world when it comes to helping patients develop lifetime strategies to avoid ever developing chronic pain related to common non-traumatic causes. We are the posture and movement specialists in the healthcare world and our patients are looking for our expertise.
Dr. Brian Jensen is a graduate of Palmer Chiropractic College and owner of Cave Spring Chiropractic in Roanoke, VA He has been in practice for over 35 years. As a member of the Foot Levelers Speakers Bureau, he travels the country sharing his knowledge and insights. See continuing education seminars with Dr. Jensen and other Foot Levelers Speakers at footlevelers.com/continuing-education-seminars.
References
1. (Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States, 2016 Weekly / September 14, 2018 / 67(36);1001—1006 James Dahlhamer, PhDl; Jacqueline Lucas, MPH1; Carla Zelaya, PhDl; Richard Nahin, PhD2; Sean Mackey, MD, PhD3; Lynn DeBar, PhD4; Robert Kerns, PhD5; Michael Von Korff, ScD4; Linda Porter, PhD6; Charles Helmick, MD7 (VIEW AUTHOR AFFILIATIONS))
2. https://www.health.harvard.edu > mind-and-mood > depression-and-pain
3. https://www.who.int/news/item/...
4. https://drugabusestatistics.or...
5. Clinical Chiropractic (2006) 9, 59—69
 View Full Issue
View Full Issue