Melatonin administration may reverse the nociceptive threshold in spinal nerves.
In fact, researchers refer to melatonin receptors as 'a novel target’ in supporting neuropathic pain.
Pain is both a cause and consequence of sleep deficiency and sleep deficiency is both a cause and consequence of pain. So, it makes sense that melatonin would be a good support nutrient for pain because of this bidirectional association, and it is. What is surprising, however, is that several other interesting melatonin pathways affect nociception and unveil a major clinical relevance. Melatonin has always been a helpful supplement for addressing sleep deficiency, but recent research demonstrates that exploring the other mechanisms related to pain (other than correcting sleep patterns) can improve outcomes for patient management.
Melatonin and Sleep: Melatonin is a derivative of serotonin; it is a neurohormone synthesized and secreted mainly by the pineal gland (although also secreted by the GI tract, lungs, renal cortex, and eye retina) and uses tryptophan as a precursor. It is involved in the regulation of circadian and biological rhythms and the associated physiological responses such as sleep, anxiety, and pain. Proper sleep is a necessity for everyone, but even more so for those who consider sleep a struggle. For fibromyalgics, for instance, the less they sleep, the less growth honnone they produce during the night, the less repair that happens to muscle and connective tissue micro-tears, hence more pain. The pain then causes less sleep, and the vicious cycle is set in motion. Utilizing melatonin as a support supplement for fibromyalgics would seem like a good idea, and in fact there is research (including clinical trials) confirming the premise (Caumo W, et at). Low melatonin is a biomarker of circadian dysregulation and also the pain cycle is correlated to major depression and fibromyalgia symptom severity. J Pain Res. 2019; 12:(545-556.); Hussain SA, et al. Adjuvant use of melatonin for treatment of fibromyalgia. J Pineal Res. 2011;50(3):)267-271.) Melatonin is a useful support nutrient for aiding sleep patterns and contributing to the pain cycle in this sense. However, discussing the multiple ways in which melatonin is related to pain, other than through sleep, can shed light on developing protocols for positive outcomes.
Direct Effects on Nociception: One
of the most direct effects of melatonin is on membrane and nuclear receptors, and this contributes to its purported anti-nociceptive properties. Chen, WW et al. 2016 reported melatonin-mediated effects via its MT1/MT2 receptors at the dorsal hom levels of the spinal cord and interactions with p-endorphins, in addition to receptors that included opioid, GABA, substance P and NMDA (N-Methyl-D-aspartate). Melatonin is reported to be effective support in many of these cases “as an anxiolytic and analgesic agent, indicating its clinical application” (Chen WW, et al. Pain control by melatonin: Physiological andpharmacological effects. Exp TherMed. 2016 Oct; 12(4): 1963-1968; Lopez-Canul M, et al. Selective melatonin MT2 receptor ligands relieve neuropathic pain through modulation of brainstem descending anti-nociceptive pathways. Pain. 2015;156(2):305-317). Melatonin was associated not only with the pain threshold but also the threshold of thermal hypersensitivity; there is also evidence supporting the hypothesis that melatonin affects cyclooxygenase-2 (COX-2), the enzyme responsible for inflammatory prostaglandins and leukotrienes (ibid., Chen, W. et el. 2016).
Direct Receptor Effects on Nociception Defined:
Beta endorphins: are neuropeptide hormones involved in natural reward circuits and the perception of pain. They are produced in certain neurons within the nervous system. Opioid receptors: modulate substances that act on pain. GABA receptors: respond to the inhibitory neurotransmitter GABA, widely known as a calming agent. Substance P: is a neuropeptide acting as a neurotransmitter and neuromodulator; it is found in the brain and spinal cord and is associated with pain and inflammation. NMDA: NMDA receptor pathways participate in the transmission of pain, and melatonin is considered to affect hypersensitivity and tolerance by suppressing NMDA receptor activities in the spinal cord.
Melatonin as an Antioxidant: Melatonin acts as a free radical scavenger during inflammation and injury, reducing nuclear factor-kappa B (NF-kB) and cytokines IL-6 or TNF-a, which all contribute to inflammation and pain (Xie S, et al. Role of Melatonin in the Regulation of Pain. JPain Res. 2020 Feb 7:13:331-343). It is well-accepted that pain and anxiety interact with each other. Xie S. et ah 2020 note the efficacy of melatonin in an analgesic and anxiolytic role, and “given these properties with few adverse side effects, melatonin has potentiaF’... for patient management.
Melatonin Epigenetic Influences on Pain: Accumulating evidence suggests that enviromnental demethylation of the Tetl gene (Tetl) is associated with nociception hypersensitivity; however, melatonin inhibits Tetl expression, leading to methylation enrichment and low expression of glutamate receptors in dorsal horn neurons, and subsequently a favorable effect on neuropathic pain (Chen WW, et al. Pain control by melatonin: Physiological and pharmacological effects. Exp Ther Med. 2016 Oct;12(4): 1963-1968).
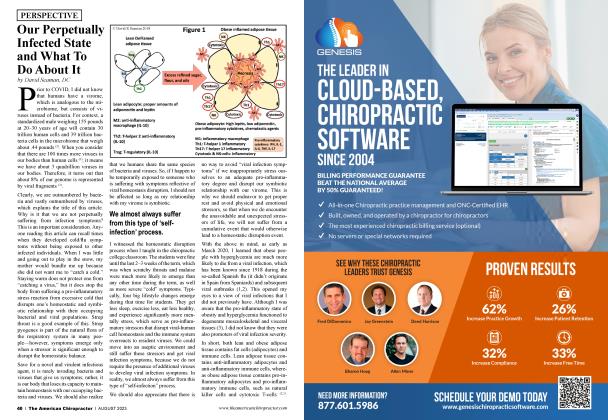
These very powerful acupuncture pointscan be used for multiple applications. They represent either the Beginning of an Acupuncture Meridian or the End of one.
The multifactorial facets of melatonin and its effects on pain and anxiety deserve speculation on how this supplement fits into patient treatment protocols.
Moreover, melatonin has been reported to help support allodynia (sensitive nerve pain). This epigenetic, anti-nociceptive effect of melatonin was believed to involve enhancement of gene expression in neurons (Lin TB, et al. Melatonin reliex’es neuropathic allodynia through spinal MT2-enhanced PP2Ac and downstream ELD AC4 slmttling-dependent epigenetic modification ofhmgbl transcription. J Pineal Res. 2016:60(3):263-276).
Support for Specific Scenarios:
GI tract: The gastrointestinal system creates and releases almost a 400-fold higher amount of melatonin than the pineal gland (without circadian rhythms like the pineal body). Involvement of the central nervous system in the action of melatonin on irritable bowel syndrome has been suspected by researchers, and in fact scientific trials have demonstrated a positive supportive effect on irritable bowel syndrome (Mozaffari S, et al. Implications of melatonin therapy in irritable bowel syndrome: A systematic review. Curr Pharm Des. 2010:16:3646-3655: Lu WZ. et al. Melatonin improves bowel symptoms in female patients with irritable bowel syndrome: A double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2005:22:927-934). Additionally, melatonin’s supportive effect on anxiety can benefit IBS patients.
Surgery Support: Surgery anxiety is known to aggravate postoperative pain. A recent systematic meta-analysis study that included 24 studies with a total of 1,794 patients suggested that melatonin impacted the preoperative anxiety score and postoperative pain score, as compared with placebo (Comai S, et al. Melancholic-like behaviors and circadian nenrobiologicalabnormalities ... Int JNeuropsychopharmacol. 2015:18(3):pyn0 75-pyuO 75).
Headache: “A meta-analysis of current trials of phannacotherapy for cluster headache suggests that 10 mg of melatonin daily could be given,” both during and before the headache manifests for good support (Francis GJ, #66 as cited byXie et at. 2020 op. cit.).
Neuropathic: Melatonin administration may reverse the nociceptive threshold in spinal nerves. In fact, researchers refer to melatonin receptors as “a novel target” in supporting neuropathic pain (Xie S, et at. 2020 op. cit.).
In conclusion, melatonin should not be classified strictly as a nutrient that helps regulate circadian rhythms and facilitate sleep patterns. The multifactorial facets of melatonin and the different pathways it affects just in the realm of pain and anxiety deserve speculation on how this supplement fits into patient treatment protocols.
Clinical AK testing for Melatonin Insufficiency by Stephan Ediss DC:
There are a number of reasons why patients lose sleep (overstimulation by blue light, inappropriate neurologic response to ocular exposure to light, poor microbiota, old trauma, circadian rhythm, low levels of melatonin, etc.). During a patient evaluation, assessment can be perfonned to ascertain possible causes of sleep interruption/deprivation. For the purposes of this article, our focus will be on low or lack of melatonin and how to assess. Through muscle-response testing, we can challenge the patient’s neurologic response to the light and darkness. With the patient supine, a strong muscle test should stay strong with exposure to light or exposure to darkness. Typically, when a patient goes weak in the dark, it is an indicator of the aforementioned possibilities of sleep pattern disturbances. With the lights off, if the doctor places their hand over the patient’s abdomen and it causes a weak muscle to become facilitated again, it can be an indicator of a melatonin issue. Using a weak muscle test with the lights off, involvement of acupuncture meridians can be evaluated by touching the beginning and endpoints (B & E Points) on the patient’s face. Involved acupuncture meridians will facilitate a weak muscle test in the dark. Muscle testing the patient with a quality melatonin product may facilitate a weak muscle in the dark, indicating the need for melatonin supplementation. Because of the relationship between melatonin and the gut, in particular the microbiome, challenging the patient for probiotics is also recommended. Once the appropriate nutritional support and dosage has been determined, neurologic corrective measures can be taken. While the patient lays their hands over the small intestine, the doctor taps the involved B & E points (roughly 100 times) and then perfonns an injury recall technique (IRT) with the patient’s hands still over the small intestine. A follow-up patient progress and assessment should be performed within a week of this procedure.
Dr. Lynn Toohey organizes seminars, acts as a nutritional consultant to Nutri-West (www.nutriwest. com) and authored the Functional Health Evaluation program that analyzes blood tests and DNA raw data (www.FHEcloud.com). Dr. Toohey can be reached at [email protected] with any questions.
Stephan P. Ediss, DC, PAK, FIACA, has over 300 hours of certified training as a professional applied kinesiologist and has been in practice for 31 years. All his knowledge is compiled in an organized, easy-to-follow, step-by-step protocol resulting in amazing clinical outcomes. Call him at 307-358-3147 or email at [email protected].
 View Full Issue
View Full Issue