I’VE WRITTEN MANY ARTICLES OVER THE PAST YEARS discussing the symptoms associated with degenerative disc disease and the utilization of nonsurgical spinal decompression (NSSD). During our latest course, we talked about failed back surgery syndrome and how the odds keep diminishing for positive results after the first procedure.
Tiger Woods has undergone another surgery for his lower back. It was his sixth surgery, and his timetable to return to golf is unclear.
Woods’ social media accounts announced that the 15-time major winner visited the hospital for a special surgery in West Palm Beach, Florida — a microdecompression surgery of the lumbar spine for nerve impingement.
In a statement, Woods stated, “The surgery went smoothly, and I’m hopeful this will help alleviate the back spasms and pain I was experiencing throughout most of the 2024 season. I look forward to tackling this rehab and preparing myself to get back to normal life activities, including golf.”
I have met Tiger Woods, a true gentleman, and sat with him along with Jack Nicklaus and President Donald Trump. His back muscles were amazing. He discussed how rehabilitation was very important for him to continue playing golf.
However, in my humble opinion, the fact that he has had six surgeries while in phenomenal shape shows that exercise and rehabilitation are not always the answers. Doctors, our time as back and disc specialists is now. I am confident that there is a need for nonsurgical spinal decompression and that spinal surgery is not always the answer.
Dr. Bard and I now have 245 clinics in 45 states and Canada. I am excited that week after week, we get letters from doctors with great testimonials from patients about how they are no longer in pain and no longer facing back surgery.
Dr. Bard and I have worked with and learned fiom Dr. Norman Shealy, MD, PhD, who is probably the most published in the world on NSSD, and other medical leaders. Dr. Shealy told Dr. Bard and me that he knew that back surgery was not the answer.
Dr. Glen Zuck is an orthopedic surgeon who once worked with the Philadelphia Eagles. He said, “I would never hesitate to refer to a Disc Centers of America doctor. They understand the spine and the disc and provide an alternative to surgery.”
I’ve been in this profession for 40 years. There was a time when medical doctors did not refer to chiropractors, but the tide changed. Now is the time for us to step up and move forward as leaders in the treatment of back pain and disc disease.
Some surgeons have stated that “80 to 85% of the time, although they can visualize an anomaly on the X-ray or MRI, they cannot, with any certainty, determine the source of the pain.” That’s why 10 spine surgeons will propose 10 different solutions; one may recommend fusing the spine at three levels, while another sees no indication for any type of procedure. The ambiguity inherent in diagnosing back pain makes it possible for surgeons to do anything they want.
Dr. Richard Deyo reported, “Chronic back pain is among the most common patient complaints, and its prevalence and impact have spawned a rapidly expanding range of tests and treatments. Some of these have become widely used for poorly validated indications, leading to uncertainty about efficacy and safety, increasing complication rates, and marketing abuses.
Dr. Deyo masterfully weaves together the science, business, and politics of treatment for an ailment that has bedeviled humankind throughout recorded history. He tells the story of America’s best and brightest, President John F. Kennedy among them, who succumbed to interventions that caused more harm than good.
Watch Your Back! is a page-turning guide for the afflicted and those who seek to help them heal. In the book, Dr. Deyo tells the appalling, infuriating, and outrageous tale of how money and poor science helped turn the United States into the back surgery capital of the world. This book is essential reading for anybody with a spinal column.
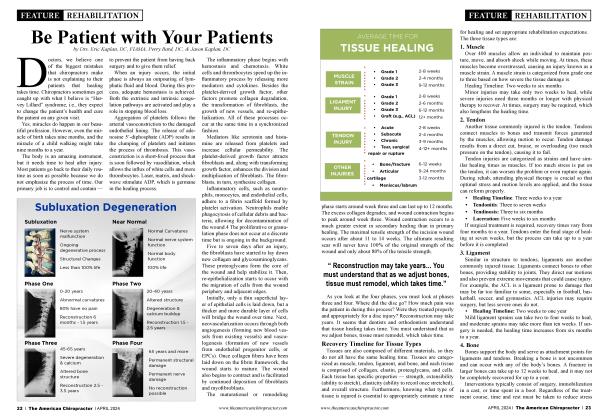
Data on the causes of failed back surgery is limited. Among orthopedists, there is a consensus that the timing of recurrent symptoms provides information helpful for diagnosis.1 Immediately after surgery, failure to achieve relief of symptoms or a continuation of preoperative symptoms has been attributed to an initial wrong diagnosis, technical error, or poor patient selection because of psychosocial factors.
Temporary relief after surgery followed by pain recurrence within a few weeks of surgery suggests infection. When pain occurs months after surgery, reherniation, battered root syndrome (inflammation of the nerve root because of surgical manipulation), epidural fibrosis, or arachnoiditis are suspected. Failures after several years may be caused by loss of spinal instability or spinal stenosis, either at the previous surgical site or at an adjacent level.
“That’s why 10 spine surgeons will propose 10 different solutions; one may recommend fusing the spine at three levels, while another sees no indication for any type of procedure”
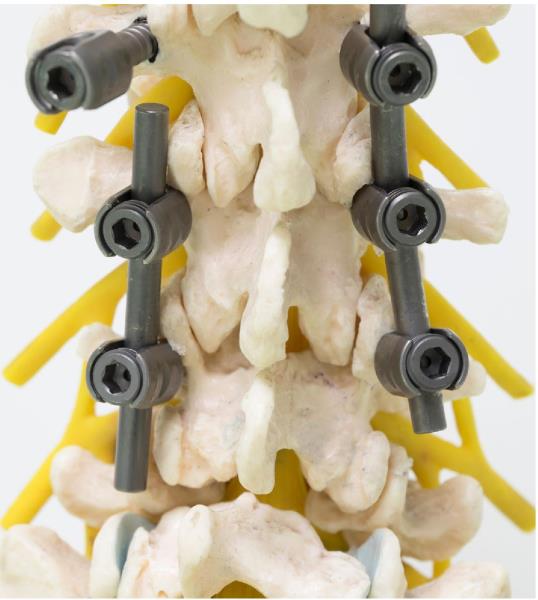
Loss of stability can result from excessive bone removal during decompression surgery. For instance, resection of 50% or more of the facet joint affects the stability of the spine.8 Spinal instability also can occur at an adjacent level after fusion surgery because of increased motion as the adjacent segments compensate for the loss of motion at the fused segment.
“Some authors have suggested that the cause of ongoing back pain in patients with failed back surgery syndrome may be possible to diagnose in as many as 90% of patients”
Spinal instability increased from 12% after one operation to 50% after four or more revision surgeries in one retrospective study.1 Risk factors for reoperation are spinal fusion with surgery, being older than 60, and workers’ compensation claims.5 Some authors have suggested that the cause of ongoing back pain in patients with failed back surgery syndrome may be possible to diagnose in as many as 90% of patients.9
I love working with medical doctors, and we also work and teach with Dr. Robert Burke, one of the most talented radiologists I have ever met. He refers many medical doctors to DCOA clinics.
The epidemic of back pain costs and expenditures amazes me. Recent studies document a 629% increase in Medicare expenditures for epidural steroid injections. Epidural injections that are not FDA approved for back pain are important to me. A 423% increase in expenditures for opioids for back pain scares me.
Our job as chiropractors and wellness providers is to try to keep people from becoming opioid and drug dependent. Dr. Burke and Dr. Zuck have discussed the complications after surgery by developing adhesions that couple to the spinal nerves, creating chronic pain.
What do other MDs think about surgery? At the 2010 American Academy of Orthopedic Surgeons conference, 100 surgeons were polled about whether they’d personally have lumbar spinal fusion surgery for unspecific low back pain. All but one answered “absolutely not.”
However, even today, back surgery is growing in record numbers in our country. Surgery is big business often governed by greed. Patients who have not done well are referred to return to the operating room repeatedly, losing ground after each procedure. About one in five patients who undergo spinal surgery for a degenerative disorder return for a revision procedure — a second operation.
Even when the fusion is deemed to be “radiologically perfect” — meaning that an X-ray shows the vertebrae have grown together and the hardware is positioned correctly — the fusion itself imposes increased stress on other vertebral segments. That often results in “adjacent segment deterioration,” a condition where the vertebral level above or below degrades, causing more pain. A second back surgery only has a 30% chance of success, and that prognosis drops to 15% for a third back surgery with 5% for a fourth.
Oregon Health and Science University spine medicine researcher Roger Chou believes that surgeons should be required to reveal the odds to their patients before going forward. “If [the surgeon] said, ‘Yes, we can do this $70,000 surgery, but you know, there’s still more than a 50% chance that you’re going to have a lot of pain. And you still won’t be able to work. You’re going to still need pain medicine. You’ll have complications related to the surgery. All of this is well documented.’ Then most people would say, T don’t want it.’”
I have previously noted that approximately 30% of my patients have had surgery. In an article in a medical trade journal, orthopedic surgeon Terry Amaral made a note of some things that can go wrong that are rarely mentioned to surgical candidates.
“The spinal cord is right next to where we are putting the screws in; we are working near where the nerve roots exit,” he observed. “If you perforate that area, the patient will experience weakness or even paralysis. Then, in the front of the spine, there are other things to be concerned about, like the aorta, the vena cava, the lungs.”
Why did they vote against surgery? The answer is simple: often, the risk-reward ratio just wasn’t good enough. So, why do surgeons continue to pursue this type of operation if the success rate is often below 50%?
According to Hyan Bae, who conducts research for Cedars-Sinai Medical Center, failed back surgery is alarming. “They have their own inherent conflict,” said Bae. The prominent orthopedic surgeon further explained, “It’s not only a financial conflict. It’s an emotional conflict. We get paid to do the work. We want to make the patient better. So we concentrate on the good results, and we dismiss the bad results.”
Bae added that surgeons cannot be held entirely responsible because they are under constant pressure from patients who beg them to “do something.” Under these circumstances, it’s hard not to want to be a hero, but often, recovery stalls within weeks even if the procedure goes well.
The American Journal of Medicine observed that about 80,000 spine surgeries fail annually in the United States alone, which is a disturbing number. So why don’t more choose nonsurgical spinal decompression as a treatment option? Simply because many doctors buy tables to make money without fully understanding the science and research behind this revolutionary technology.
Despite risks and mediocre outcomes, the number of spinal fusions performed in the United States grew from 61,000 in 1553 to more than 465,000 in 2011 — more than a 600% increase, accounting for more than 60% of the spinal fusion surgery performed worldwide. It’s the most expensive form of elective surgery in the United States, costing about $40 billion annually.
For 20 years, the Dartmouth Atlas of Health Care Project (dartmouthatlas.org) is a study that has documented variations in how medical resources are allocated in the United States. In 2011, the university’s Institute for Health Policy and Clinical Practice, which produces the atlas, reported a puzzling finding. The prevalence of spine surgery in Casper, Wyoming, was nearly six times higher than it was in the Bronx, New York. Even more baffling, the rate in St. Cloud, Minnesota, was twice that of Rochester, Minnesota, the home of the Mayo Clinic, only 150 miles away.
I had the opportunity to talk with one of the leading orthopedic surgeons in the U.S., Dr. Timothy Kremchek. He often discusses how he had back surgery and regrets it because he’s been suffering ever since. He says he’d recommend nonsurgical spinal decompression before any type of invasive procedure (even an epidural) because there is no downside. As I’ve stated in past articles, you can watch Dr. Kremchek talk about back surgery on my son’s website, Wellingtondisccenter.com — look for it under medical reviews.
Although there are exceptions, most European and UK surgeons avoid the procedure, while U.S. surgeons are quick to operate and fuse the spine. Oxford University Hospital’s orthopedic surgeon Jeremy Fairbank stated, “I end up sending most of my patients with chronic pain to rehabilitation programs and, therefore, end up fusing a tiny number of highly motivated patients. If you have a spinal fusion operation, you are off work for four to eight weeks and sometimes longer. A rehab program takes one to three weeks.” Lumbar spinal fusion is an operation with a tainted reputation.
Let’s review: approximately 80% of adults experience lumbar pain at least once in their lifetime, and 80% of structures cause lumbar pain. We now are confident that this pain may often be related to intervertebral discs. A subluxation becomes a bulge, and a bulge a herniation. Our role is to treat the disc before it ruptures.
Disc herniation is multifactorial and frequently related to degenerative processes and mechanical effects. It mostly occurs because of external injuries of the spine, such as spinal bending and stretching, spinal rotation exercises, and abrupt posture changes.
Both surgical and conservative treatment methods are considered for intervertebral disc herniation. Our goal with NSSD is to create negative disc pressure. Negative pressure within the intervertebral disc increases its hydration and reduces pressure on the nene root by removing the force applied to the vertebral pulp. As previously discussed in prior articles by Dr. Norman Shealy and, they outlined the difference between fraction and decompression: “Eighty-six percent of ruptured intervertebral disc (RID) patients achieved ‘good’ (50-89% improvement) to ‘excellent’ (90-100% improvement) results with decompression. Sciatica and back pain were relieved. Of the facet arthrosis patients, 75% obtained ‘good’ to ‘excellent’ results with decompression.”
C. Norman Shealy, MD, PhD, and Vera Borgmeyer, RN, MA. Decompression, Reduction, and Stabilization of the Lumbar Spine: A Cost-Effective Treatment for Lumbosacral Pain. American Journal of Pain Management Vol. 7 No. 2 April 1997.
Spinal decompression therapy is now making its move in the back world. We have consistently observed how conservative treatment for intervertebral disc herniation and IDD therapy, along with decompression, is setting a new standard. Spinal decompression therapy reduces the pressure on the intervertebral disc by supplying nutrients and oxygen to it.
That creates a state of non-gravitation or negative pressure by adjusting the direction and angle of traction to suit the location of the intervertebral disc, which is the target of the treatment. This, in turn, reduces the pressure inside the intervertebral disc by gradually and softly increasing a specific part of the intervertebral disc through the decompression of a precise part of the lesion. This was first done by video fluoroscopy, which is included in the Ramos and Martin study.
“The power that creates the body has the power to heal the body.”
The Boxell and Martin study stated, “The disc has the ability to repair itself.” Is that not simply the beauty, the paradigm, the essence of chiropractic? The power that creates the body has the power to heal the body.
Patients who enter your office are often experiencing sharp, debilitating pain. This pain is not like your standard muscle soreness; in my opinion, it’s nerve pain. It’s gotten to the point where they are beginning to lose function in their daily life. They can barely make it through the workday, let alone something physically demanding, like going for a hike.
Remember the paradigm “chiropractic first, dings second, and surgery last.” It is our job as doctors and educators to make sure that the community is aware of nonsurgical spinal decompression and how we can prevent people from having back surgery.
Often, surgery is essentially an all-or-nothing event. It’s not as simple as the surgeon going in and shaving off a bit of disc or bone, sewing you up, and seeing “how you do.” A 2017 article from World Neurosurgery found that one-fifth of patients 65 and over who received a spinal surgery had to be readmitted to the hospital due to complications (Aodgwa et al. 2017).
Dr. Bard and I teach what Dr. Shealy and associates taught us. “When you reverse the load with weight on the disc, you’re increasing the disc pressure, which could create a greater chance of herniation or a sequestered disc. With decompression, the force is static unless you move. With a spinal decompression machine, the force is controlled and directed.”
Dr. Shealy and Dr. Leroy were influential in the development of a fixed tower to be more specific on the angle of the pull. The rate of application of pressure, the maximum and minimum levels of force, and the length of pressure application are all programmed into the machine. The cycling of the pressure, like a sine wave, produces a pumping action that improves circulation. This is particularly important where disc conditions are concerned since discs.
The best decompression machines are FDA-cleared and can be turned off by the patient if they have any discomfort. For most patients, decompression is so comfortable and relaxing they can take a nap during their treatment.
If you have a decompression table, you need to know what to do in a logarithmic index, a sinusoidal index, oscillation, or what algorithm the manufacturer utilizes. You will also need to have a copy of your FDA-clearance documents to look up indications of usage.
Not all tables are the same, so do your homework. Ask to see the 510 K delivered to the FDA. Also, ask to see any research done on the specific table. Dr. Shealy is adamant about marketing research on machines he works with. Do your homework; that is the job of a great doctor.
Dr. Eric Kaplan and Dr. Perry Bard, are business partners of over 32 years. They have developed Disc Centers of America & Concierge Coaches. Currently, they have over 150 clinics using their Disc Centers of America brand and lead ongoing success training events throughout the year. For more information on coaching, spinal decompression, or seminars, visit www.thechiroevent.comorwww.decompressioncertified.org, or call the Chiropractic Q&A Hotline at 888-990-9660.
Dr. Jason Kaplan is a graduate of Parker University. Along with his wife Dr. Stephanie Kaplan, they practice in Wellington Florida. Jason is an Instructor for Disc Centers of America, one of the Nation’s largest collection of doctors specializing in Disc Injuries. He has been recognized and honored by the International Disc Education Association and teaches technique at the National Certification Program at Life University and is considered a Master on Non Surgical Spinal Decompression, www.wellingtondisccenter.com.
References
1. Hazard RG. Failed back surgery syndrome: surgical and nonsurgical approaches. Clin Orthop Relat Res. 2006 Feb;443:228-32. doi: 10.1097/01.bio.0000200230.46071.3d. PMID: 16462446.
2. Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (PhilaPa 1976). 2007 Feb l;32(3):382-7. doi: 10.1097/01.hrs.0000254104.55716.46. PMID: 17268274.
3. Weir BK, Jacobs GA. Reoperation rate following lumbar discectomy. An analysis of 662 lumbar discectomies. Spine (Phila Pa 1976). 1980 Jul-Aug;5(4): 366-70. doi: 10.1097/00007632-198007000-00010. PMID: 7455766.
4. Law JD, Lehman RA, Kirsch WM. Reoperation after lumbar intervertebral disc surgery. J Neurosurg. 1978 Feb;48(2):259-63. doi: 10.3171/jns.1978.48.2.0259. PMID: 146731.
5. Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine (Phila Pa 1976). 2007 Sep 1;32(19):211926. doi: 10.1097/BRS.0b013e318145a56a. PMID: 17762814.
6. North RB, Campbell JN, James CS, Conover-Walker MK, Wang H, Piantadosi S, Rybock JD, Long DM. Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991 May;28(5):685-90; discussion 690-1. PMID: 1831546.
7. Deyo RA. Back surgery—who needs it? N Engl J Med. 2007 May 31;356(22):2239-43. doi: 10.1056/NEJMp078052. PMID: 17538083.
8. Zdeblick TA, Zou D, Warden KE, McCabe R, Kunz D, Vanderby R. Cervical stability after foraminotomy, a biomechanical in vitro analysis. J Bone Joint Surg Am. 1992 Jan;74(l):22-7. PMID: 1734010.
9. Schofferman J, Reynolds J, Herzog R, Covington E, Dreyfuss P, O'Neill C. Failed back surgery: etiology and diagnostic evaluation. Spine J. 2003 Sep-Oct;3(5):400-3. doi: 10.1016/sl529-9430(03)001220. PMID: 14588953.
10. Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA. Failed lumbar disc surgery and repeat surgery following industrial injuries. J Bone Joint Surg Am. 1979 Mar;61(2):201-7. PMID: 422604.
11. Kim SS, Michelsen CB. Revision surgery for failed back surgery syndrome. Spine (PhilaPa 1976). 1992 Aug;17(8):957-60. doi: 10.1097/00007632-199208000-00015. PMID: 1387978.
 View Full Issue
View Full Issue