Keeping Patients Safe from Sexual Predators Part 2
June 1 2024 Ben E. BenjaminKeeping Patients Safe from Sexual Predators Part 2
June 1 2024 Ben E. BenjaminSexual Assault Prevention: Keeping Patients Safe from Sexual Predators Part 2
By Ben E. Benjamin, PhD
In the previous article of this series, I covered hiring processes so that you can adhere to the safest standards of care in massage therapy. If you are interested in more detailed information or process templates, please email [email protected]. These templates will make it easier for you to do your job and provide the safest, most professional environment.
Suggested for a sidebar: For chiropractors who hire massage therapists, it is paramount to protect your patients and business from inappropriate sexual behavior, which results in thousands of reports every year. These recommendations and guidelines come from someone with 20 years of experience as an expert witness, a PhD in sports medicine, and over 50 years of experience in the massage industry.
6. Draping Personal Areas
Draping means that the areas of the body not being treated are completely and securely covered with a sheet. If a patient complained that they felt exposed in a session — their sheet felt loose, or they were concerned their breasts or genitals were going to be exposed — consider this a warning sign that a therapist may have acted inappropriately.
Many patients, especially new ones, are not clear about what constitutes appropriate draping. The practitioner is responsible for using proper draping to ensure that their patients feel secure without fear of exposure. In most sexual abuse cases I have worked on, the predatory therapist knew how to drape appropriately but chose not to with a particular patient.
 Image 1
Image 1
 Image 2
Image 2
The genital region should always be covered (Image 1). In Image 2, you can see that the drape may be lowered to the base of the sacrum when the patient is prone. The buttocks may be undraped only with explicit permission from the patient and only one side at a time (Image 3). When putting the drape in place (as in Image 1), the therapist may lift the leg slightly to bring the drape securely under the thigh. While the patient is disrobed, the legs should never be spread wide apart to secure the drape.
The primary fact to remember is that the drape exists to define the area of the body to be treated. The therapist’s hands should never go under the drape.
Sensitive Regions of the Body
The Female Breasts
The female breasts should always be fully draped, not partially covered. When the patient is supine, the drape generally covers the body up to the shoulders when the arms are under the drape and to the upper axilla when the arms are on top of the drape (Images 4a and 4b). Sometimes, the drape is lowered one or two inches to work on the upper pectoral muscles, but only when the patient gives explicit permission.
 Image 4
Image 4
A potentially legitimate reason for working near the breast is the treatment of injuries to the intercostal muscles, which can benefit from various forms of hands-on therapy. The same can be true for the pectorals and other types of tissue damage in close proximity to the breast (Image 5). Intercostal massage is appropriate only when performed by a therapist trained in working with these particular types of injuries, and only after the specific request of a patient seeking help for this issue.
Warning Sign: Touching the Breasts in the Prone Position
When a patient is lying prone on the table, there is never a legitimate reason for the therapist to make contact with her breasts. Often, when a woman lies prone, the sides of her breasts extend out to the side, so it takes conscious awareness and care to avoid touching them.
 Image 5
Image 5
When working on the patient’s back, a therapist may knowingly (with malicious intent) or unknowingly (because of poor training) bring their hands close to the treatment table and run them over the sides of the breasts. That is never acceptable. When the therapist’s hands move down from the top of the patient’s shoulders and return to the low back, they should be on the edges of the back but never low enough to touch the sides of the breasts. (Images 6 and 6a)
 Images 6 and 6a
Images 6 and 6a
 Images 6 and 6a
Images 6 and 6a
If the therapist touches the sides of the breast, the patient may feel confused about what happened. In many of the abuse cases I see, the victim reports wondering whether the touch was accidental, intentional, or something she imagined.
Breast Massage (or treatment under or near breast tissue)
Most massage therapists trained in the United States are not qualified to perform breast massage, but some have had quality training or postgraduate education. A woman may have several reasons for wanting to have breast massage or injury treatment near or under the breast tissue — a painful, clogged milk duct for a mother breastfeeding; a painful post-mastectomy scar; a strained lower pectoral muscle that goes under the breast; or strained intercostal muscles. In most states, breast massage is not legal. If it is legal in your state, it should only be performed with written informed consent.
The Upper Inner Thighs
It is also essential to maintain good physical boundaries during thigh massage. The upper inner thigh is often a very private, sexually sensitive area. The drape should always cover the upper three to four inches of the inner thigh, whether the patient is supine or prone.
In most massage therapy sessions, the therapist should never touch the very upper inner thigh (Image 7). Careless technique is no excuse for the fingers to move under the drape near the genital region. This will make patients uncomfortable and should never happen.
 Image 7
Image 7
The only exceptions to these guidelines occur when the patient specifically requests therapeutic work on an injury in this region. For example, a patient may seek treatment for a strained upper adductor muscle-tendon unit from a therapist who is trained in working with those injuries, or the chiropractor may request that the patient receive this type of treatment. This therapeutic treatment should only be performed with written informed consent.
The Lower Abdomen
Abdominal massage can be very therapeutic for certain conditions, including constipation and injuries to various abdominal muscles. However, the abdomen — especially the lower abdomen — is a very sensual area of the body for most of the population. From my experience as an expert witness, I am aware that lower abdominal massage is often a precursor to a predator therapist moving his hands increasingly lower and in a sexualized way.
 Image 8
Image 8
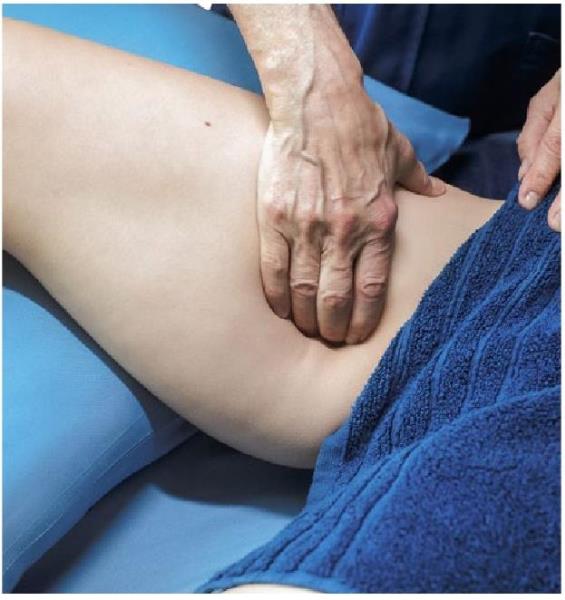 Image 8
Image 8
As a rule, the therapist’s hands should remain at least two inches above the patient’s pubic bone. Depending on the patient’s build, this boundary will lie roughly two to three inches below the navel. There may be some exceptions to this guideline, such as the treatment of Caesarean section scars or similar surgical scars by a qualified therapist trained in scar tissue work. If the therapist has a good therapeutic reason to perform abdominal massage, it should be explained, and they should receive the patient’s written informed consent before the treatment begins.
 Image 9
Image 9
Sometimes, legitimate accidents do occur. One real example, cited in a book I coauthored with Cherie Sohnen-Moe, The Ethics of Touch (Sohnen-Moe Associates, 2013), occurred when a chiropractor found himself in an unfortunate situation that was quickly and easily dealt with through honest and direct communication:
A male chiropractor was beginning to work on a prone female patient who was wearing a gown opened in the back. He placed one of his hands on her lower legs and the other hand on her upper back. Suddenly, with a cry of shock, the patient said, “Doctor, what’s going on?” The chiropractor looked down and saw that his tie had fallen between the patient’s thighs. In an even and professional voice, he said, “I’m sorry; my tie slipped and is touching you. Let me keep my hands where they are while you turn your head to see for yourself.” The patient saw that the chiropractor was telling the truth; because of his clear and honest communication, she relaxed and continued the treatment. (4)
In the case of honest error, as this example illustrates, the therapist immediately stops, apologizes, and provides a direct, straightforward explanation of what has happened. If anything sexually inappropriate occurs more than once by a practitioner, it is likely intentional sexual misconduct, and the practitioner should no longer see patients. It is the practitioner’s and clinic’s responsibility to ensure that patients are protected from any inappropriate sexual contact.
The Genital Region
The genital region should never be touched in a massage session under any circumstance, even by accident. I am familiar with multiple cases of fingers repeatedly touching or brushing against a woman’s labia, as well as being inserted into the vagina. In almost every case I have testified in, the woman freezes the moment the abuse occurs and is unable to move or say anything. At this point, they are experiencing sexual trauma and often go into shock. A predator therapist may incorrectly interpret this reaction as agreement with what is being done when actually the patient is frozen in fear. After experiencing such abuse, these women may suffer from extreme emotional distress. In the overwhelming majority of cases I’ve seen, the woman reported an inability to have sexual contact with her partner for years after the violation. Any touching of the patient’s genital region during a massage, even by accident, is never acceptable.
7. Code of Ethics
Adopt a code of ethics that includes explicit statements that no sexual contact of any kind can occur between the practitioner and the patient and include it within your new hire training manual. Each therapist should read and sign a copy to be kept in their employment file. Also, display the code of ethics so that it is visible, such as in the break room if you have one. This establishes safety and acts as a deterrent, as well as being a signal to employees that your business values and upholds ethical behavior.
For reference, some massage organizations that include a clear statement about sexual contact in their code of ethics are the American Massage Therapy Association (AMTA), Associated Bodywork and Massage Professionals (ABMP), College of Massage Therapists of Ontario (CMTO), and the National Certification Board of Therapeutic Massage and Bodywork (NCBTMB).
8. Zero Tolerance
Have a brief yet explicit “zero tolerance” statement regarding sexual assault or harassment of patients and colleagues in the workplace. Having a series of unambiguous statements about unacceptable actions and behaviors makes your values and policies resoundingly clear. Each hired therapist should read and sign the statement in front of the owner or manager, which will be added to their employment file. (A sexual misconduct statement template is available by email.)
All-Staff Zero-Tolerance Meetings
Whenever an accusation or complaint of sexual assault, verbal impropriety, or inappropriate physical contact is reported to a chiropractic clinic, a general meeting of the entire staff and therapists should be called as soon as possible. To protect the privacy of all concerned, the names of patients or therapists involved in the incident are never mentioned in these meetings.
These mandatory emergency meetings let all employees know that your organization truly enforces their zero-tolerance policies, and they reinforce all written policies that may be overlooked or ignored over time. They also create a greater sense of safety for everyone. An atmosphere of openness and honesty must be encouraged by the organization’s management and leaders to have an effective sexual assault prevention policy.
If a patient initiated the inappropriate incident, they should have been permanently banned already. If the accused was a therapist, they should already be suspended from working at the office pending an investigation and should not be present at this meeting.
The alleged incident should be described by management in detail to all attendees. Employees are asked to come forward at that time, privately afterward, or anonymously with any information that they may have about this or any other incident they know of where a therapist or patient has been inappropriate. They should also be encouraged to reach out to you or the manager or file an anonymous report at any time they become aware of any such behaviors — not just in response to a meeting. Otherwise, employees often never say anything and inappropriate incidents go uninvestigated or completely unreported. (A sample meeting agenda outline template is available by email.)
9. Supervision
Sometimes, a massage therapist has an uncomfortable or disturbing experience when giving a patient a massage. The patient may have made an off-color joke or was more subtly inappropriate. Practitioners need a shame-free, trustworthy relationship with a supervisor to review and evaluate such challenging or difficult experiences.
Supervision can occur in small groups or in one-on-one sessions. There are two types of supervision: technical and relationship or clinical supervision. A technical supervisor can help guide therapists to develop their hands-on techniques. A relationship or clinical supervisor helps practitioners learn how to define their own boundaries, set boundaries for challenging patients, and deal with any intense feelings or sexual attraction that may develop. Offering both clinical and technical supervision for your therapists by a qualified practitioner is an asset to your business and a deterrent to underlying personal and professional conflicts. (Supervision models are available by email.)
About the Author
Dr. Ben E. Benjamin holds a PhD in sports medicine and has been an expert witness in cases of sexual assault in the massage and bodywork field since 2004. He is the coauthor of The Ethics of Touch, a textbook used in schools throughout North America to teach ethics and boundaries to massage therapists and other hands-on healthcare professionals. In 1974, Dr. Benjamin founded the Muscular Therapy Institute, a school he owned and directed for over 30 years. In the 1980s, he developed a 150-hour curriculum in ethics and communication skills for therapists in training. He has also taught courses in ethics, boundaries, and communication to somatic therapists for over 30 years. In addition to his work with pain and injury problems, he did much pioneering work in the areas of ethics and communication, including writing articles on professional, sexual, and business ethics.
Dr. Ben E. Benjamin holds a PhD in sports medicine and has been an expert witness in case. In 1974, Dr. Benjamin founded the Muscular Therapy Institute, a school he owned and directed for over 30 years. In the 1980s, he developed a 150-hour curriculum in ethics and communication skills for therapists in training. In addition to his work with pain and injury problems, he did much pioneering work in the areas of ethics and communication, including writing articles on professional, sexual, and business ethics. For more information visit www.BenBenjamin.com
 View Full Issue
View Full Issue