DOCTORS, THERE HAS NEVER BEEN A BETTER TIME FOR CHIROPRACTIC THAN TODAY. But as the world is changing, we need to accelerate our advanced knowledge of the spine and spinal decompression. We, as professionals, should be leaders in disc care and the treatment of bulging and herniated discs, and we should help the public avoid unnecessary surgeries.
Why is decompression so important? Because it is our job to help patients avoid back surgery. Dr. Norman Shealy, MD, PhD, said, “After my first back surgery, I knew surgery was not the answer.” Dr Bard, myself, and our sons have worked diligently with neurosurgeon Dr. Norman Shealy, truly understanding spinal decompression’s dynamics and the future.
With that said, according to MedReport, it is estimated that 200,000 Medicare patients with back pain underwent $2 billion worth of unnecessary surgeries, including spinal fusion and/or laminectomy or vertebroplasty, over a recent three-yearperiod, based on analysis of Medicare claims data from the Lown Institute.
We’ve contacted many surgeons and orthopedic surgeons. One who lectures the National certification, Dr. Glenn Zuck, who also worked with the Philadelphia Eagles, understands the value of decompression. According to Dr. Timothy Kremcheck, one of the nation’s leading orthopedic surgeons we spoke with, “The risk of surgery is enormous.”
Imagine then unnecessary; such procedures put patients at risk of blood clots, pneumonia, heart and lung issues, infections, paralysis, and death. After surgery, 10% to 40% of patients experience “failed back surgery syndrome,” in which the vertebrae do not fuse back together, the report said. “The times in which spinal fusion and laminectomy work for spinal stenosis are when the stenosis is causing neurogenic claudication, or radicular symptoms, meaning you’re getting pain shooting down the leg; the nerve is pinched,” Vikas Saini, MD, president of the Lown Institute, told MedPage Today.
“But if you don’t have that... and you just have spinal stenosis without that pain, then those surgeries are not effective.”
Spinal fusion is recommended for patients with low back pain caused by traumatic injury, sciatica, slipped spinal bone, or spinal deformity. The report excluded spinal fusion/laminectomy surgeries from those considered unnecessary if the claim documented radicular symptoms, trauma, herniated disc, discitis, spondylosis, myelopathy, radicular pain, scoliosis, neural claudication, or spondylolisthesis. His report states, “For patients who have low back pain caused by aging, there is not sufficient evidence of a benefit from these procedures compared to nonsurgical alternatives,” the report noted.
There has never been a better time for Chiropractic than today. The Lown Report folly illustrates the fraud and abuse that is taking place regarding back surgery today. Failed back surgery is now considered a syndrome more than a diagnosis. The alternative spinal decompression. With NSSD, Nonsurgical Spinal decompression, we work to get negative disc pressure and spinal distraction without muscle contraction, as outlined in the Ramos and Martin study.
According to the Lown Report, Vertebroplasty procedures were defined as overused for patients with spinal fractures caused by osteoporosis. Patients with bone cancer, myeloma, or hemangioma were excluded from those considered to have undergone unnecessary procedures. When the Lown Institute removed claims for which there was good reason for the surgery, “we are still left with a lot of unnecessary cases,” Saini said.
When Saini was asked if surgeons or the people who submitted claims on their behalf could have made mistakes, been lazy, or not checked the right ICD-10 diagnosis codes, he noted that there could have been some of that, but not nearly in the numbers that the institute found.
Saini was also asked why Medicare would pay for procedures without diagnostic justification. “The answer about why Medicare pays is because Medicare doesn’t use appropriateness criteria to decide whether to pay,” he replied. “Maybe that’s the real big story here. Why does the Lown have to do this? Because nobody else does.”
The Lown report does not name the surgeons performing these potentially unnecessary procedures. Still, it does draw an association between large sums of money paid by the spine surgery industry to surgeons “with measurable spinal fusion/ laminectomy or vertebroplasty overuse.” For example, “NuVasive and Medtronic paid physicians $8 million and $7.5 million, respectively, from 2020 through 2022.”
Charles Rosen, MD, of the University of California Irvine, and a specialist in spine surgery who was not involved in producing the report, found its conclusions credible. It captures “the practice of operating on low back pain without any of the qualifiers that indicate a legitimate need for surgery — neurogenic compression or compression of the nerve, scoliosis, spondylolisthesis, tumor, [or] fracture,” he told MedPage Today. “It’s not accepted in academic circles to operate on just back pain or discogenic disease when you have no real etiology for the pain,” he said.
As I continued to read the report, I was amazed at how difficult Medicare can be for the chiropractic industry. It seems the surgical industry gets a free pass. I am grateful to doctors like Dr. Marty Kotlar from Target Coding, who work diligently to provide Coding and compliance to doctors throughout the country. At Disc Centers of America, we recommend Dr. Kotlar and pay for his initial consultation with our clients.
As I continued with the report, it stated, “Dr. Rosen also echoed Saini’s comment that Medicare just pays for everything. “It’s called pay-and-chase. They approve everything, and that’s where the huge amount of abuse for Medicare comes in.”
He noted that several studies have shown that losing weight, stopping smoking, and engaging in healthier activities are better treatments for back pain when the patient doesn’t have a specific diagnosis, like nerve compression or deformity.
I learned from this report the enormous costs of back surgery. If so, that makes Nonsurgical Spinal Decompression very cost-effective. There is a reason many doctors want to add hardware to any back surgery. DR. Rosen also pointed to the heavy influence that the spine surgery equipment industiy has on hospitals and surgeons. “I mean, spinal hardware is $1,000 a screw, and you put in three or four levels, you can get $20,000, $30,000 of equipment put in.” In the report, the hospitals with the highest rates of unnecessary spinal fiisions/laminectomies included:
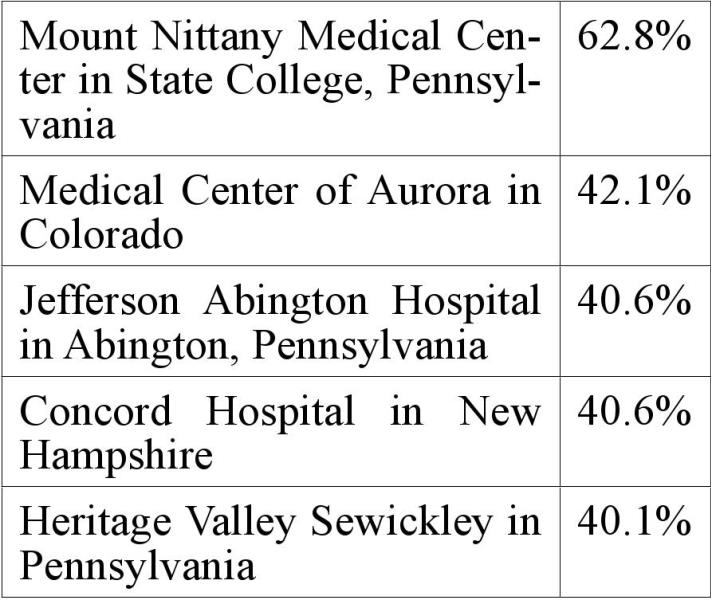
Hospitals with high rates of unnecessary vertebroplasty included:
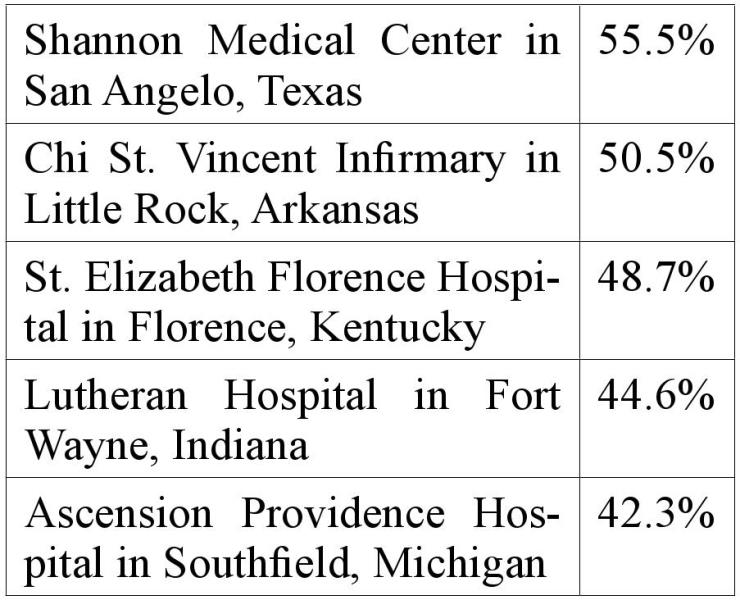
The report also named hospitals with low rates of unnecessary spinal fusion/ laminectomy procedures, which included Avala Hospital in Covington, Louisiana (0.1%); Northwest Specialty Hospital in Post Falls, Idaho (1.2%); Fresno Surgical Hospital in California (1.2%); Baylor Surgical Hospital at Las Colinas in Irving, Texas (1.3%); and Christus Mother Frances Hospital in Tyler, Texas (1.7%). Several hospitals had no claims for unnecessary vertebroplasty procedures, including MetroHealth Medical Center in Cleveland, Essentia Health - St. Joseph’s Medical Center in Brainerd, Minnesota; Marshall Hospital in Placerville, California; and Denver Health Main Campus in Colorado.
As I continued to read this report, which correlates with Dr. Richard Deyo’s report out of Washington, I noticed a wide variation in unnecessary procedures from state to state. The report stated, “For example, hospitals in New Hampshire, Iowa, Massachusetts, Pennsylvania, Alabama, and Hawaii had the highest average rates of unnecessary spinal fusion/laminectomy procedures, while Arkansas, Kansas, Oklahoma, Nevada, Nebraska, and Indiana had the highest average rates of unnecessary vertebroplasty procedures.” How was this calculated, you may ask?
“For the report, overuse was measured using Medicare fee-for-service claims data from 2020 to 2022, and Medicare Advantage claims data from 2019 to 2021. The cost of unnecessary back surgeries was calculated using Medicare’s procedure price lookup tool for outpatient procedures, using the most frequent Current Procedural Terminology code for the procedure. The cost of inpatient procedures was calculated using the average Medicare cost of the most frequent Diagnosis Related Group code for the procedure, using Medicare feefor-service claims data.” He also stated:
“I found it amazing that the report noted that none, zero, of the hospitals contacted for comment responded as of press time.”
The medical profession now goes on defense regarding back surgery. Our role now should be to go on offense to prevent unnecessary back surgery. As we teach DISC CENTERS of America doctors, you must explain to patients to include in every report findings that back surgery can be unnecessary and provide this report, this article, as a guideline to helping them make an educated decision. Dr. Perry Bard and I, along with our sons Dr. Jason Kaplan & Dr. Devin Bard, work with doctors all the time, providing them with research not only on the success of nonsurgical spinal decompression but also explaining to them the consequences of back surgery that have the potential of Failed back surgery.
The best way to get medical referrals is to get them from the patient’s primary carrier before they are recommended to a surgeon. Here is a letter that we provide our doctors to utilize.
Leg pain is one of the most common associated symptoms seen in lower back injuries. Leg pain can occur in different patterns depending on its origin in the lower back. Generally, pain radiated to the leg is divided into two main categories. The first category is called radicular pain and is the direct result of spinal nerve compression that supplies the leg. Radicular pain is well understood and is the category that testing such as myelograms and CAT scans detect. This is why diagnostic testing is so important and creating a positive decision on choosing nonsurgical spinal decompression before any surgery.
The second categoiy is referred to as joint pain. Referred leg pain follows less specific patterns than does radicular or nerve pain. It is, however, overwhelmingly the most common type of leg pain, and it accompanies back injuries. Thomas N. Bernard and William H. Kirkaldy-Willis, M.D. Professor of Orthopedic Surgery at the University of Saskatoon, Canada, studied 1293 cases of low back pain.1 They found that referred leg pain was twice as common as nerve pain. Referred pain to the leg occurs secondary to joint pain in the lower back. Interestingly, Drs. Bernard and Kirkaldy-Willis also found that spinal manipulation or chiropractic treatment was most effective for low back pain and referred to leg pain. 452 of their patients had a good treatment result with spinal manipulation, more than with any other treatment tested in the group of 1293 patients. Other treatments in their study included injections, conservative medical treatment, and surgery.
Dr. Kirkaldy-Willis, in another large study, found chiropractic manipulation to be very successful with low back and referred leg pain 2 In that study, he suggests that few medical doctors will have the time or inclination to master the art of spinal manipulation and that they should refer them to a practitioner skilled in this treatment, such as a chiropractor. He says, “The physician who makes use of this resource will provide relief for many patients.” This report is very beneficial and can be downloaded and provided for your patients. With research showing that the majority of low back injuries are joint injuries with referred pain syndromes and that spinal manipulation is the most appropriate treatment, chiropractors will be more frequent participants in work and accident-related low back pain cases. Often, your diagnostics will show a disc injury. Whether it is a bulge, a herniation, or if there are annular tears.
These studies above should highlight the positive aspects of Chiropractic and potential side effects of back surgery. At DCOA, Dr. Bard and I believe you need to provide these studies to the patients, which is why we wrote thebestdiscbook. com. Clinical studies have shown Decompression Therapy to be highly effective in treating back pain. In a recent study published in Orthopedic Technology Review, Decompression Therapy was shown to be 86% effective in treating herniated and degenerative discs. Another study published in Anesthesiology News showed that after 4 years, over 91 % remained pain-free.
Here are some other studies that show just how effective decompression therapy is:
• In the Journal of Neurological Research vol. 20, no. 4, April 1998, the researchers stated: “We consider decompression therapy to be a primary treatment modality for low back pain associated with lumbar disc herniation at single or multiple levels, degenerative disc disease, facet arthropathy, and decreased spine mobility. Physiology (pain and mobility) and pathology correlate imprecisely. We believe that post-surgical patients with persistent pain or ‘Failed Back Syndrome’ should not be considered candidates for further surgery until a reasonable trial of decompression has been tried.”
• In the Journal of Neurological Research vol. 23, no. 7, October 2001, the researchers stated: “For any given patient with low back and referred leg pain, we cannot predict with certainty which cause has assumed primacy. Therefore, surgery, by being directed at root decompression at the site of the herniation alone, may not be effective if secondary causes of pain have become predominant.
• Decompression therapy, however, addresses both primary and secondary causes of low back and referred leg pain. We thus submit that Decompression therapy should be considered first, before the patient undergoes a surgical procedure which permanently alters the anatomy and function of the affected lumbar spine segment.”
• In the same Volume of the Journal of Neurological Research, the Senior Lecturer in Orthopedics at Sydney University stated, “Successful reduction of intradiscal pressures with decompression therapy represents a technological advance in lumbar spinal treatment and is likely to affect both the biomechanical and biochemical causes of discogenic pain.
Clinical studies have shown that Nonsurgical Spinal Decompression Therapy is extremely effective in treating back pain. In a recent study published in Orthopedic Technology Review, Decompression Therapy was shown to be 86% effective in treating herniated and degenerative discs. Another study published in Anesthesiology News showed that after 4 years, over 91 % remained pain-free.
Decompression therapy should be considered first before the patient undergoes a surgical procedure, an invasive procedure that permanently alters the anatomy and function of the affected lumbar spine segment.
In Review, Spinal Decompression has been cleared by “The Food and Drug Administration”. You’ve gotten to know them as the “FDA” 51 OK. The main conditions treated with Non -surgical spinal decompression, which has documented success, are:
• Back pain
• Sciatica
• Herniated and/or bulging discs (single or multiple),
• Degenerative disc disease,
• A relapse or failure following surgery.

Dr. Eric Kaplan and Dr. Perry Bard, are business partners of over 32 years. They have developed Disc Centers of America & Concierge Coaches. Currently, they have over 150 clinics using their Disc Centers of America brand and lead ongo www.thechircevent.com on coaching, or www.decompressioncertified.org, spinal decompression, or seminars, or call visit the Chiropractic ing success training events throughout the year. For more information Q&A Hotline at 888-990-9660.

Dr. Jason Kaplan is a graduate of Parker University. Jason is an Instructor for Disc Centers of America, one of the Nation’s largest collection of doctors specializing in Disc Injuries. He has been recognized and honored by the International Disc Education Association and teaches technique at the National Certification Program at Life University and is considered a Master on Non Surgical Spinal Decompression, www.wellingtondisccenter.com.
References
1. Bernard TN, Kirkaldy-Willis WK. RECOGNIZING SPECIFIC CHARACTERISTICS OF NONSPECIFIC LOW BACK PAIN. Clinical Orthopedics And Related Research, 1987;217:266-280.
2. Kirkaldy-Willis WH, Cassidy ID. SPINAL MANIPULATION IN THE TREATMENT OF LOWBACK PAIN. Canadian Family Physi1985;31:535-540.
 View Full Issue
View Full Issue